Intentional self-harm hospitalisations
Why are rates of intentional self-harm hospitalisations important?
Intentional self-harm and suicide are significant public health issues in Australia (AIHW: Harrison and Henley 2014). Intentional self-harm is associated with a number of interacting factors that are related to individual mental health, family and social circumstances. Social risk factors that have been identified for adolescent suicide include parental separation, divorce and family discord, as well as child abuse, bullying and peer victimisation (Brodsky et al. 2008; Klomek et al. 2008). This is also the time in life when many mental illnesses develop and young people have the highest incidence of diagnosable symptoms of mental illness (ABS 2008; Patel et al. 2007), which may increase the risk of suicidal intentions and behaviour.
Do rates vary across population groups?
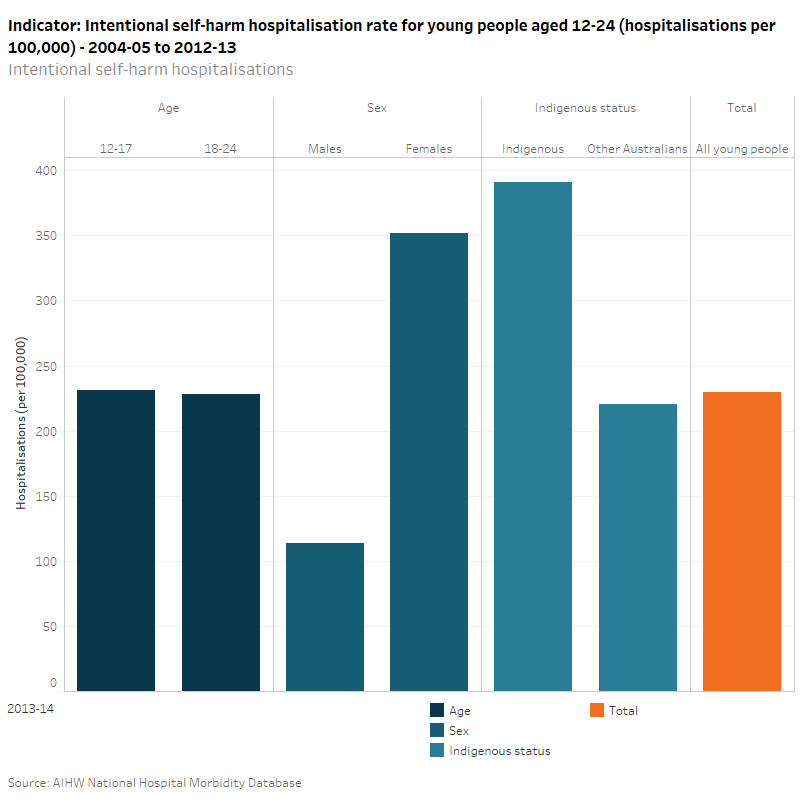
In 2013–14, the rate of hospitalisations due to intentional self-harm among all young people aged 12–24 in Australia was 230 per 100,000. Young people aged 12–17 had a slightly higher rate (232 per 100,000) of intentional self-harm hospitalisation than those aged 18–24 (229 per 100,000). Females had a much higher rate of hospitalisation than males, with 352 per 100,000 and 114 per 100,000, respectively. Indigenous young people were almost twice as likely to be hospitalised due to intentional self-harm (391 per 100,000) as Other Australian young people (220 per 100,000).
Has there been a change over time?
There has been a gradual increase in hospitalisation rates for all young people aged 12–24 from 188 per 100,000 in 2007–08, to 230 per 100,000 in 2013–14. This appears to be largely driven by a steep increase in hospitalisation rates for youths aged 12–17 from 139 per 100,000 to 232 per 100,000, over the same period. In contrast, there are no strong trends observed for intentional self-harm hospitalisation rates for young people aged 18–24, with rates remaining steady at 230 per 100,000.
There has been a notable increase in hospitalisation rates for young females from 267 per 100,000 in 2007–08, to 352 per 100,000 in 2013–14. There is no clear trend in the intentional self-harm hospitalisation rate for males with rates of around 115 per 100,000 from 2004–05 to 2013–2014.
For young Indigenous Australians, the rate of intentional self-harm hospitalisations has grown considerably from 240 per 100,000 in 2006–07, to 391 per 100,000 in 2012–13. The rate for Other Australian young people has been markedly lower than Indigenous Australians over this period and has largely mirrored the trend observed for all young people aged 12–24.
Injury hospitalisations are coded based on principal diagnosis, using the ICD-10-AM range S00-T75 or T79. Cases using this criterion are referred to as community injury. In 2013–14, diagnoses and external cause injury and poisoning were recorded using the 8th edition of the ICD-10-AM. Data from 2004–05 to 2012–13 were coded to earlier editions.
Intentional self-harm hospitalisations includes injury cases in which the first reported external cause is in the ICD-10-AM range X60-X84 as per AIHW: Pointer S 2013. Trends in hospitalised injury, Australia, 1999–00 to 2010–11. Injury research and statistics series no. 86. Cat. no. INJCAT 162. Canberra: AIHW.
Hospitalisations (referred to elsewhere as hospital separations) refer to episodes of admitted patient care which can be a total hospital stay or a portion of a hospital stay, beginning or ending in a change of type of care (for example, from acute care to rehabilitation). To reduce over-counting of injury cases, records have been omitted where the mode of admission is recorded as a transfer from another acute-care hospital.
Indigenous data is for 6 States (NSW, Vic, Qld, WA, SA and public hospitals in the NT) as these states are considered to have sufficient completeness of Indigenous identification for analysis from 2004–05 onwards. ACT and Tasmania are considered to have sufficient completeness of Indigenous identification from 2010–11 onwards; however, they are excluded for the purposes of time series analysis. Consequently, the Indigenous data may not necessarily be representative of the excluded jurisdictions.
Changes in the quality of the Indigenous identification over time may affect the time series for data presented for data by Indigenous status (i.e. categories ‘Indigenous’ and ‘Other Australians’).
‘Other Australians’ includes records for persons identified as not Indigenous as well as records where Indigenous status was not stated.
The hospitals admitted patient care data do not include non-admitted presentations to hospital (eg non-admitted patients in emergency departments).
AIHW National Hospital Morbidity Database
Data quality statement: AIHW METeOR
ABS 2008. National Survey of Mental Health and Wellbeing: summary of results, 2007. ABS cat. no. 4326.0. Canberra: ABS.
AIHW: Harrison JE & Henley G 2014. Suicide and hospitalised self-harm in Australia: trends and analysis. Injury research and statistics series no. 93. Cat. no. INJCAT 169. Canberra: AIHW.
Brodsky BS, Mann JJ & Stanley B 2008. Familial transmission of suicidal behaviour: factors mediating the relationship between childhood abuse and offspring suicide attempts. Journal of Clinical Psychiatry 69:584–96.
Klomek AB, Marocco F & Kleinman M 2008. Peer victimisation, depression and suicidality in adolescents. Suicide and Life-threatening Behaviour 38(2):166–80.
Patel V, Flischer AJ, Hetrick S, & McGorry P 2007. Mental health of young people: a global public-health challenge. The Lancet 369 (9569): 1302-1313.


