Cervical screening (PI22)
This indicator is the proportion of female First Nations regular clients aged 25–74 who have not had a hysterectomy and who had a cervical screening test within the previous 5 years.
It is collected for females in age groups:
- 25–34
- 35–44
- 45–54
- 55–64
- 65–69
- 70–74.
There have been changes to the specification of this indicator over time. For more information see Interpreting nKPI data.
Why cervical screening is important
Cervical screening aims to detect and treat precancerous abnormalities that might otherwise progress to cervical cancer. First Nations women generally experience a high burden from cervical cancer compared with non-Indigenous women (AIHW 2021).
The National Cervical Screening Program (NCSP), which aims to reduce mortality from cervical cancer, was originally targeted at women aged 20–69 for a 2-yearly Papanicolaou (Pap) smear, or ‘Pap test’, to detect precancerous abnormalities of the cervix. From 1 December 2017, the NCSP changed to 5-yearly cervical screening for women aged 25–74 using a primary human papilloma virus (HPV) test with partial HPV genotyping and reflex liquid-based cytology triage.
While the HPV vaccine is very effective at protecting against the 2 most common cervical cancer-causing types of HPV, it doesn’t protect against all types of HPV that can lead to cervical cancer. This means that both HPV-vaccinated and unvaccinated women are recommended to have regular Cervical Screening Tests (the Pap test replacement) to reduce their risk of developing cervical cancer.
At June 2023, 42% (or around 45,300) of female First Nations regular clients aged 25–74 who have not had a hysterectomy had a cervical screening test within the previous 5 years (Figure 1).
Figure 1: Cervical screening within the previous 5 years by reporting period
Cervical screening within the last 5 years by reporting period
This Tableau visualisations shows the percentage of female First Nations regular clients aged 25–74 who have not had a hysterectomy in the last 5 years, for reporting periods from December 2020 to June 2023 for either:
- type of organisation (ACCHO, non-ACCHO)
- remoteness area (Major cities, Inner regional, Outer regional, Remote, Very remote)
- state/territory (NSW/ACT, Vic, Qld, WA, SA, Tas, NT)
- age (age group 25–34, 35–44, 45–54, 55–64, 65–74).
Data supporting this visualisation are available in Excel supplementary data tables at Data.
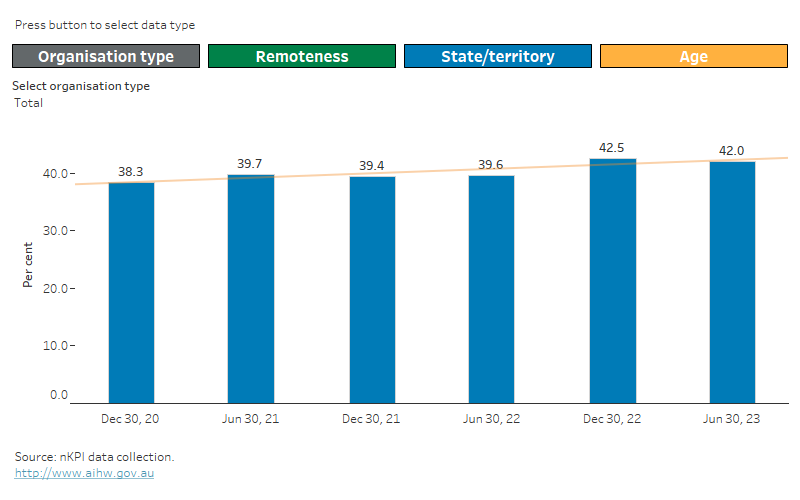
Note: For more information, including on interpreting changes over time, see Technical notes.
For more information on cervical screening see Data.
Reference
AIHW (Australian Institute of Health and Welfare) (2023) National Cervical Screening Program monitoring report 2023, Cancer series 141. Cat. no. CAN 157, AIHW, Australian Government, accessed 2 January 2024.


