Medicare-subsidised mental health-specific services
In 2021–22, almost 2.8 million people (11% of Australians) accessed 13.6 million Medicare-subsidised mental health-specific services.
49% of services were provided by psychologists, 27% by GPs and 19% by psychiatrists in 2021–22.
31% of services were delivered via telehealth in 2021–22.
In 2021–22, the number of people receiving services and the number of services delivered was highest in the July–September and lowest in the January–March.

Medicare-subsidised mental health‑specific services are delivered by psychiatrists, general practitioners (GPs), psychologists and other allied health professionals. These services are delivered in a range of settings – for example, hospitals, consulting rooms, home visits, and telehealth – as defined in the Medicare Benefits Schedule (MBS). Information is provided on both patient and service provider characteristics and is limited to Medicare-subsidised services only. These data relate only to services claimed under specific mental health care MBS item numbers. Therefore, the reported number of patients is unlikely to represent all patients who receive mental health care as it is unclear how many people receive GP mental health-related care that is billed as a consultation against, for example, a general MBS item number. For further information on the MBS data, refer to the data source section.
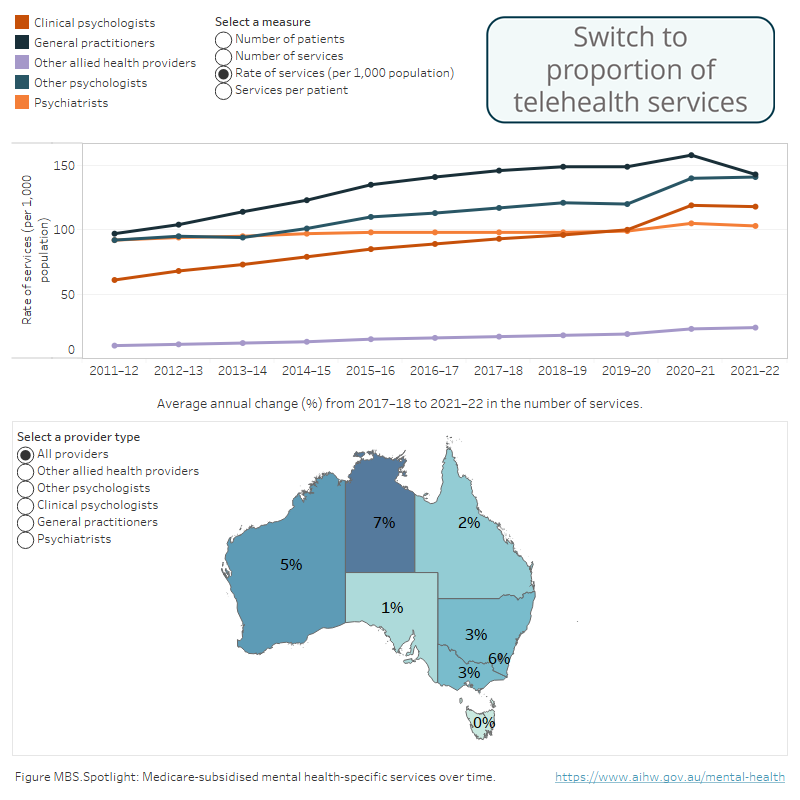
During 2021–22, the Medicare-subsidised mental health-specific service rate was 529 services per 1,000 population in Australia with the highest rate provided by General practitioners (143).
Spotlight data
Has the provision of Medicare-subsidised mental health-specific services increased over the past 10 years?
Has the provision of Medicare-subsidised mental health-specific services increased over the past 10 years?
Infographic containing an overview of medicare-subsidised mental health-related services over time that include number and rates of patients and services by provider type.
Source: Medicare-subsidised mental health-related services 2021–22 tables: Table MBS.11
Who received Medicare-subsidised mental health-specific services?
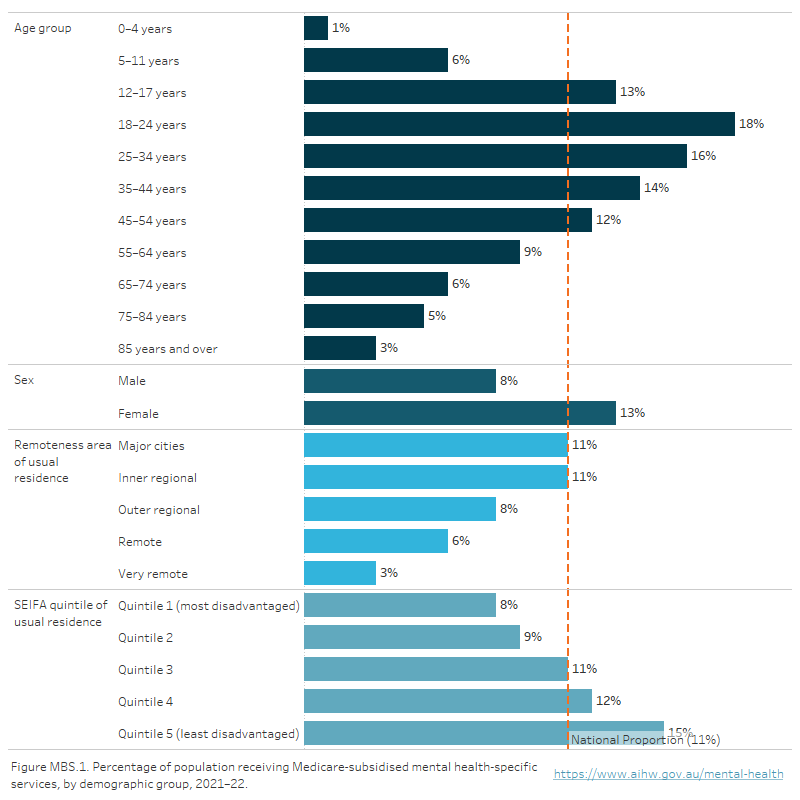
In 2021–22, 2.8 million Australians (11% of the population) received Medicare-subsidised mental health-specific services with Victoria having the highest rate (12%) and the Northern Territory the lowest (6%).
People aged 18–24 years were most likely to receive services (18% of people aged 18–24 years) and females had a higher rate (13%) compared with males (8%) (Figure MBS.1). The rate of receiving services decreased with increasing remoteness. In Major cities and Inner regional areas the rate was 11% decreasing to 3% in Very remote areas. People living in the least disadvantaged SEIFA quintile were the most likely to receive services (15%) decreasing to 8% for people in the most disadvantaged quintile.
Figure MBS.1: Rate (per 100 population) of people receiving Medicare-subsidised mental health-specific services, by demographic characteristics, 2021–22
Horizontal bar chart showing the percentage of the population who received Medicare-subsidised mental health-specific services during 2021–22, by key demographics. In 2021–22, the service users increased with age from 1% of people aged 0–4 years, to 18% of patients aged 18–24 years. It then gradually decreases for older age groups from 12% for 45–54 years to 3% for those aged and 85 years and over. A greater proportion of the female population (13%) received services compared with males (8%). For remoteness area, the same proportion of people living in Major cities and Inner regional areas (11%) received services while services received decreased as remoteness increased: Outer regional (9%), Remote (6%) and Very remote (3%). Refer to Table MBS.2.
Source: Medicare-subsidised mental health-related services 2021–22 tables: Table MBS.2
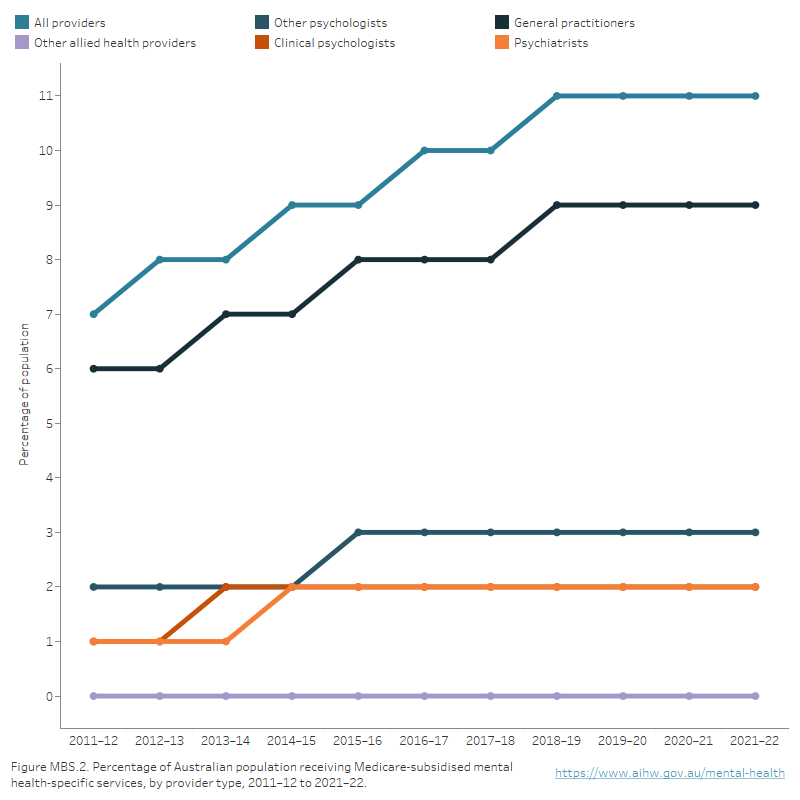
In 2021–22, 9% of the Australian population received services from a General practitioner; 5% for psychology services; 2% from a Psychiatrist; and <1% received services from Other allied health professionals. Note that an individual may receive services from more than one provider type. The General practitioners section provides further information about mental health-related GP care.
Over time
The number of people receiving services increased from 1.6 million in 2011–12 (or 7% of the population) to 2.8 million in 2021–22 (11% of the population). Increases were seen for all provider types, with the greatest increase occurring for General practitioners (from 6% to 9%). The proportion of Australians accessing Clinical psychologist services increased from 1% in 2011–12 to 2 in 2021–22 in line with those receiving Psychiatrist MBS services (Figure MBS.2).
Figure MBS.2: Percentage of Australian population receiving Medicare-subsidised mental health-specific services, by provider type, 2011–12 to 2021–22
Line chart showing the percentage of Australians receiving Medicare-subsidised mental health services by provider from 2011–12 to 2021–22. The percentage of Australians receiving services from psychiatrists increased from 1% in 2011–12 to 2% in 2021–22, GPs increased from 5% to 9%, clinical psychologists 1% to 2%, other psychologists 2% to 3%, and other allied health providers 0% to 1%. The percentage of Australians receiving services from all providers increased from 7% in 2011–12 to 11% in 2021–22. Refer to Table MBS.4.
Source: Medicare-subsidised mental health-related services 2021–22 tables: Table MBS.4
Other allied health providers include mental health professionals such as occupational therapists, social workers, Aboriginal health workers, and mental health nurses. From 2011–12 to 2021–22, the number of people receiving Medicare-subsidised mental health-specific services from other allied health providers has increased at a higher rate than other types of providers.
The average annual change of people receiving medicare-subsidised mental health specific services from 2017–18 to 2021–22 was 5% for other allied health providers (noting that less than 1% of the population received these services between 2017–18 and 2021–22), and ranged between 1% and 5% for other types of providers. Similarly, among all service providers, the average annual change for the number of services delivered was highest for other allied health providers from 2017–18 to 2021–22 (10%, compared to a range of 2% to 7% for other providers). This increase of service may be partially driven by the increase of other allied health providers supplying service (12% average annual increase from 2017–18 to 2021–22).
General practitioners (GPs) are often the first point of contact for people seeking mental health care services. GPs provide a variety of services to people with a mental illness and may refer patients on to specialised services.
There were 2 data sources up until 2016 that provided complimentary insights into mental health-related GP care: the Bettering the Evaluation and Care of Health (BEACH) survey of general practice activity and the mental health-specific Medicare Benefits Schedule (MBS) items which are reported in this section. For further information on the BEACH survey refer to the data source section.
Mental health-specific services
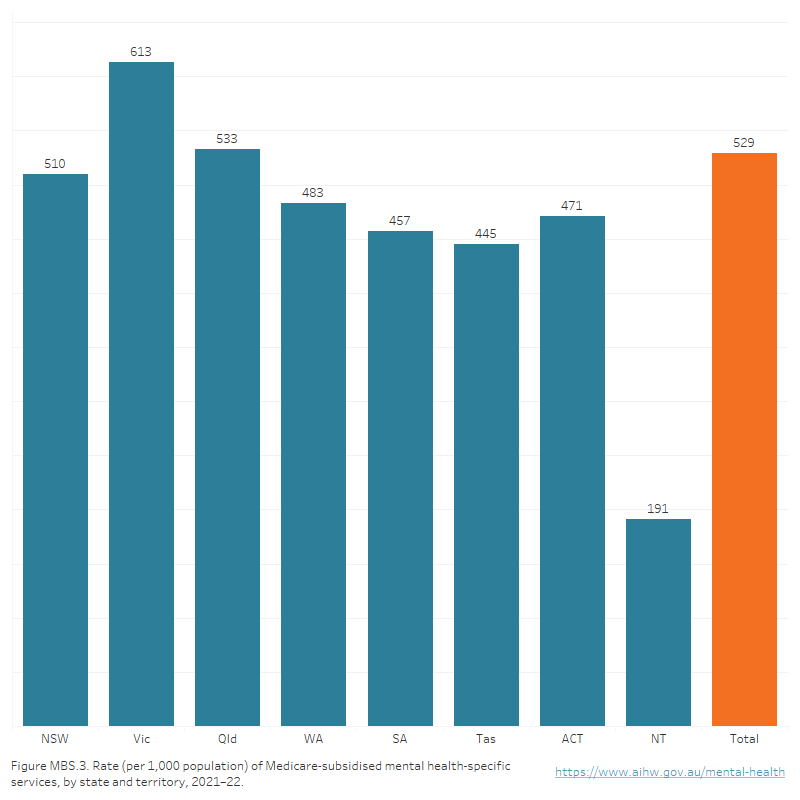
How many Medicare-subsidised mental-health services were provided?
There were 13.6 million Medicare-subsidised mental health-specific services provided to 2.8 million Australians in 2021–22. Victoria had the highest rate (613 services per 1,000 population) and the national rate was 529 (Figure MBS.3).
Figure MBS.3: Rate (per 1,000 population) of Medicare-subsidised mental health-specific services, by state and territory, 2021–22
Vertical bar chart showing the Medicare-subsidised mental health-specific service rate (per 1,000 population), by states and territories in 2021–22. Victoria (613) and Queensland (533) had the highest rate of services per 1,000 population, greater than the national rate (529). In the other states and territories, New South Wales had 510 services per 1,000 population, followed by Western Australia (483), Tasmania (445), the Australian Capital Territory (471), South Australia (457), and the Northern Territory (191). Refer to Table MBS.12.
Source: Medicare-subsidised mental health-related services 2021–22 tables: Table MBS.12
In 2021–22, the 18–24 age group had the highest rate of service use (91 services per 100 population), and females (70) had a higher rate of service use than males (36). People living in Major cities had the highest rate of service use (58) with rates decreasing with increasing remoteness. Similarly, people in the least disadvantaged SEIFA quantile had the highest rate of service use (85) with rates decreasing with increasing disadvantage (Figure MBS.4).
Figure MBS.4: Rate (per 100 population) of Medicare-subsidised mental health-specific services, by demographic group, 2021–22
Horizontal bar chart showing the rates of Medicare-subsidised mental health services per 100 population by key demographics in 2021–22. Service use in 2021–22 was lowest among patients aged 0–4 years (2 services), and increased with age with the highest for those aged 18–24 years (91), then gradually decreased for older age groups: 25–34 years (81), 35–44 years (69); 45–54 years (59), 55–64 years (47), 65–74 years (30), 75–84 years (20), and 85 years over (11). By sex, females accessed a greater number of services than males (70 compared with 36 respectively). For remoteness area, the highest service rate was seen in Major cities (58 per 100 population) with service rates decreasing as remoteness increased: Inner regional (47), Outer regional (33), Remote (19) and Very remote (10). Refer to Table MBS.10.

Source: Medicare-subsidised mental health-related services 2021–22 tables: Table MBS.10
Average number of services per patient
In 2021–22 the average number of services per patient was 5 nationally. This was consistent across all states and territories except for the Northern Territory which had the lowest number of services per patient at 3. People aged 12–74 years had the highest average number of services per patient (5) and females (5) had more services per patient than males (4).
Over time
The total number of Medicare-subsidised mental health-specific services increased from 7.9 million in 2011–12 to 13.6 million in 2021–22; an increase from 352 services per 1,000 population to 529 (Figure MBS.5). This was mainly due to increases in services provided by GPs, followed psychologists. From 2011–12 to 2021–22 there was a relatively small increase in the rate of these services delivered by psychiatrists. From March 2020 new MBS items were added in response to the COVID-19 pandemic, including an increase in the number of Better Access services available and a range of telehealth items were added across all provider types (DoH 2020).
Figure MBS.5: Rate (per 1,000 population) of Medicare-subsidised mental health-specific services, by provider type, 2011–12 to 2021–22
Vertical bar chart showing the number of services per 1,000 population for Medicare-subsidised mental health-specific services by provider from 2011–12 to 2021–22. The number of services provided by psychiatrists increased from 91 in 2011–12 to 103 in 2021–22, GPs increased from 96 to 143, clinical psychologists 57 to 118, other psychologists 95 to 141 and other allied health professionals 10 to 24. Refer to Table MBS.12.
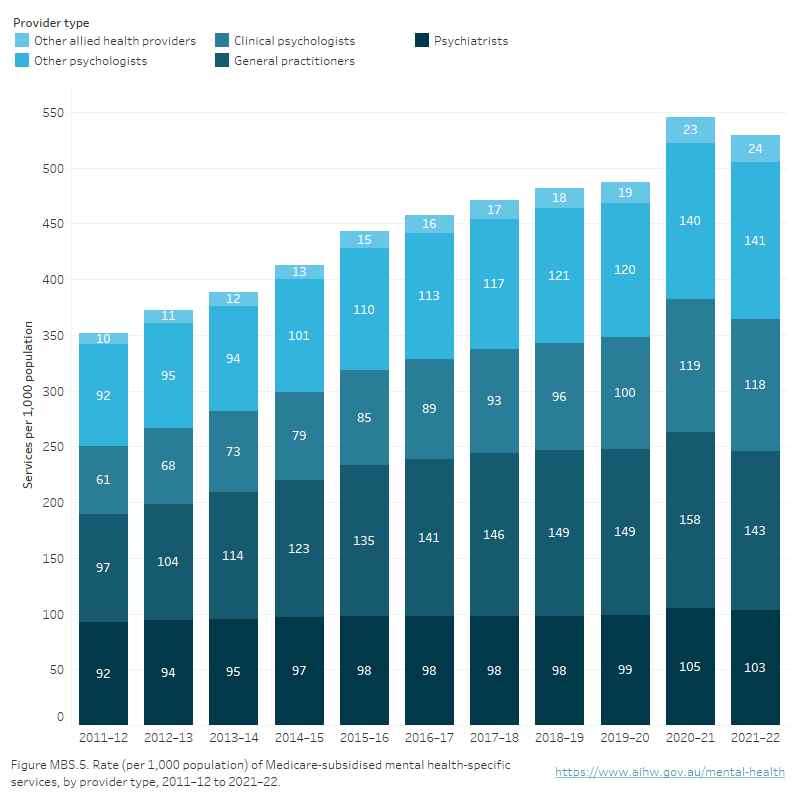
Source: Medicare-subsidised mental health-related services 2021–22 tables: Table MBS.12
How many services were provided via telehealth during the COVID-19 pandemic
During the course of the pandemic the Australian Government introduced changes to the MBS to support the provision of care via telehealth, to help reduce the risk of community transmission of COVID-19 and provide protection for both patients and health care providers. New items added include telehealth mental health services provided by GPs, psychiatrists, psychologists and other allied health workers.
Almost 1 in 3 services (4.2 million, 31%) were provided via telehealth (phone or video) in 2021–22. Psychiatrists and psychologists provided a higher proportion of Medicare-subsidised mental health-specific services via telehealth than other types of providers (37% and 36% respectively), and GPs provided the lowest proportion (18%). More detail about the use of telehealth services during the pandemic, can be found in the Mental health services activity monitoring quarterly data.
Use of services during the COVID-19 pandemic
Analyses of the Medicare-subsidised mental health-specific services by quarter have been included to show seasonal variations in service use, and provide more insight into the impact of events such as the pandemic. These include service and person counts reported by provider type, age group and sex.
From 2012–13 to 2019–20 the number of Medicare-subsidised mental health-specific services being delivered was consistently highest in the April–June period and lowest in the October–December period (Refer to table MBS.22 for detail). Note that reduced service usage is typical during public holidays and particularly over the Christmas/New Year period.
In 2019–20, an unseasonably low number of people used services in April–June (1.2 million), likely due to the impact of the pandemic lockdown periods. However, a relatively high number of services were still used (3.2 million), meaning more services were used per person in April–June (2.7) than in other quarters (2.4).
Providers show different patterns of activity over the year. Psychologists provide services to a relatively stable number of patients, while GPs and psychiatrists showed more seasonal variations.
In 2020–21, the number of people who used services was consistent with the pattern for previous years, while in 2021–22, the number of people who used services was almost 1.3 million in the April–June quarter with almost 3.6 million services used. This represents an increase over 2019–20 but a decrease from 2020–21.
In 2020–21 the number of Medicare-subsidised mental health-specific services peaked in the July–September period (almost 3.6 million). The number of services was lower in January–March for all services apart from GPs (0.6 million for psychiatrists, 0.7 million for clinical psychologists, 0.9 million for other psychologists and 0.1 million for other allied health providers). For GPs the number of services was lowest in April–June (almost 1 million).
The number of services peaked in the July–September period at almost 3.7 million in 2021–22. The number of services was lower in January–March for all services apart from GPs (0.6 million for psychiatrists, 0.7 million for clinical psychologists, 0.8 million for other psychologists and 0.1 million for other allied health providers). For GPs the number of patients accessing services was lowest in April–June (almost 0.9 million).
Medicare Benefits Schedule data
The MBS data presented relate to services delivered on a fee-for-service basis for which MBS benefits were paid. The year and month is determined from the date the service was processed rather than the date the service was provided. Patient counts for demographic characteristics (e.g. sex, age) are derived from the last service processed in the reference period.
Services Australia collects data on the activity of all persons making claims through the MBS and provides this information to the Australian Government Department of Health and Aged Care (Services Australia 2020). Information collected includes the type of service provided (MBS item number) and the benefit paid for the service. The item numbers and benefits paid are based on the MBS (DoH 2022). Services that are not included in the MBS are not included in the data. The table below lists all MBS items that have been defined as mental health-specific.
Provider type | Item group | MBS Group | MBS item numbers |
|---|---|---|---|
Psychiatrists | Initial consultation new patient | Group A08 | 296, 297, 299, 134(a) |
Group A40 (T) | 92437, 92466(a), 92477(a), 92506(a) | ||
Patient attendances | Group A08 | 291, 293, 300, 302, 304, 306, 308, 310, 312, 314, 316, 318, 319, 320, 322, 324, 326, 328, 330, 332, 334, 336, 338, 136(a), 138(a), 140(a), 142(a), 144(a), 146(a), 148(a), 150(a), 152(a), 294(T), 288(T)(a), 353(T)(a), 355(T)(a), 356(T)(a), 357(T)(a), 358(T)(a), 359(T)(a), 361(T)(a), 364(a), 366(a), 367(a), 369(a), 370(a) | |
Group A40 (T) | 91827, 91828, 91829, 91830, 91831, 91837, 91838, 91839, 91840(a), 91841(a), 92435, 92436, 92461(a), 92462(a), 92463(a), 92464(a), 92465(a), 92475(a), 92476(a), 92501(a), 92502(a), 92503(a), 92504(a), 92505(a) | ||
Group psychotherapy | Group A08 | 342, 344, 346, 154(a), 155(a), 156(a) | |
Group A40 (T) | 92455, 92456, 92457, 92495(a), 92496(a), 92497(a) | ||
Interview with non‑patient | Group A08 | 348, 350, 352, 157(a), 158(a), 159(a) | |
Group A40 (T) | 92458, 92459, 92460, 92498(a), 92499(a), 92500(a) | ||
Case conferencing | Group A15 | 855, 857, 858, 861, 864, 866 | |
Electroconvulsive therapy | Group T01 | 14224, 153(a), 340(a), 886(a) | |
Assessment and treatment of pervasive developmental disorder (PDD) | Group A08 | 289 | |
Group A40 (T) | 92434, 92474(a) | ||
Repetitive Transcranial Magnetic Stimulation (rTMS) | Group T01 | 14216, 14217, 14219, 14220 | |
Eating Disorders Treatment Plan preparation and review | Group A36 | 90260, 90262(T)(a), 90266, 90268(T)(a) | |
Group A40 (T) | 92162, 92166(a), 92172, 92178(a) | ||
General practitioners | Mental Health Treatment Plan preparation and review | Group A07 | 281, 282, 272, 276, 277 |
Group A20 | 2715, 2717, 2710(a), 2700, 2701, 2702(a), 2712, 2719(a) | ||
Group A40 (T) | 92116, 92117, 92122, 92123, 92128(a), 92129(a), 92134(a), 92135(a), 92112, 92113, 92118, 92119, 92124(a), 92125(a), 92130(a), 92131(a), 92114, 92126, 92120, 92132 | ||
Group A42 | 93402(a), 93403(a), 93406(T)(a), 93407(T)(a), 93410(T)(a), 93411(T)(a), 93433(a), 93434(a), 93437(T)(a), 93438(T)(a), 93441(T)(a), 93442(T)(a), 93400(a), 93401(a), 93404(T)(a), 93405(T)(a), 93408(T)(a), 93409(T)(a), 93431(a), 93432(a), 93435(T)(a), 93436(T)(a), 93439(T)(a), 93440(T)(a), 93421(a), 93422(T)(a), 93423(T)(a), 93451(a), 93452(T)(a), 93453(T)(a) | ||
Mental Health Treatment service | Group A07 | 279, 894(T)(a), 896(T)(a), 898(T)(a) | |
Group A20 | 2713 | ||
Group A30 | 2121(a), 2150(a), 2196(a) | ||
Group A40 (T) | 92115, 92127, 92121, 92133 | ||
Eating Disorder Treatment Plan preparation, review and service | Group A36 | 90250, 90251, 90252, 90253, 90254, 90255, 90256, 90257, 90264, 90265, 90271, 90272, 90273, 90274, 90275, 90276, 90277, 90278, 90279(T)(a), 90280(T)(a), 90281(T)(a), 90282(T)(a) | |
Group A40 (T) | 92146, 92147, 92148, 92149, 92150, 92151, 92152, 92153, 92154(a), 92155(a), 92156(a), 92157(a), 92158(a), 92159(a), 92160(a), 92161(a), 92170, 92171, 92176, 92177, 92182, 92184, 92186, 92188, 92194, 92196, 92198, 92200 | ||
Focused Psychological Strategies | Group A07 | 283, 285, 286, 287, 371(a), 372(a), 941(a), 942(a) | |
Group A20 | 2721, 2723, 2725, 2727, 2729(T)(a), 2731(T)(a), 2733(a), 2735(a) | ||
Group A39 | 91283(a), 91285(a), 91286(a), 91287(a), 91371(T)(a), 91372(T)(a), 91721(a), 91723(a), 91725(a), 91727(a), 91729(T)(a), 91731(T)(a) | ||
Group A40 (T) | 91818, 91819, 91820, 91821, 91842, 91843, 91844, 91845 | ||
Group A41 | 93300(a), 93301(T)(a), 93302(T)(a), 93303(a), 93304(T)(a), 93305(T)(a), 93306(a), 93307(T)(a), 93308(T)(a), 93309(a), 93310(T)(a), 93311(T)(a), 93287(a), 93288(a), 93291(a), 93292(a) | ||
Family Group Therapy | Group A06 | 170, 171, 172, 996(a), 997(a), 998(a) | |
Group A07 | 221, 222, 223 | ||
Electroconvulsive therapy | Group T10 | 20104 | |
3 Step Mental Health Process | Group A18 | 2574(a), 2575(a), 2577(a), 2578(a) | |
Group A19 | 2704(a), 2705(a), 2707(a), 2708(a) | ||
Clinical psychologists | Psychological Therapy Services | Group M06 | 80000, 80001(T)(a), 80005, 80010, 80011(T)(a), 80015, 80020, 80021(T) |
Group M17 | 91000(a), 91001(a), 91005(a), 91010(a), 91011(a), 91015(a) | ||
Group M18 (T) | 91166, 91167, 91181, 91182 | ||
Group M25 | 93312(a), 93313(a), 93330(a), 93331(T)(a), 93332(T)(a), 93333(a), 93334(T)(a), 93335(T)(a) | ||
Group M27 | 93375(a), 93376(a) | ||
Eating Disorder Psychological Treatment Service | Group M16 | 82352, 82353(T)(a), 82354, 82355, 82356(T)(a), 82357, 82358, 82359 | |
Group M18 (T) | 93076, 93079, 93110, 93113 | ||
Psychologists including | Enhanced Primary Care | Group M03 | 10968 |
Focused Psychological Strategies | Group M07 | 80100, 80101(T)(a), 80105, 80110, 80111(T)(a), 80115, 80120, 80121(T) | |
Group M17 | 91100(a), 91101(T)(a), 91105(a), 91110(a), 91111(T)(a), 91115(a) | ||
Group M18 (T) | 91169, 91170, 91183, 91184 | ||
Group M26 | 93350(a), 93351(T)(a), 93352(T)(a), 93353(a), 93354(T)(a), 93355(T)(a), 93316(a), 93319(a) | ||
Group M28 | 93381(a), 93382(a) | ||
Psychology health service | Group M11 | 81355 | |
Group M29 | 93512(a), 93535(a) | ||
Group M30 | 93557(a), 93590(a) | ||
Assessment and treatment of PDD | Group M10 | 82000, 82015 | |
Group M18 (T) | 93032, 93035, 93040, 93043 | ||
Eating Disorder Psychological Treatment Service | Group M16 | 82360, 82361(T)(a), 82362, 82363, 82364(T)(a), 82365, 82366, 82367(T) | |
Group M18 (T) | 93084, 93087, 93118, 93121 | ||
Allied health providers | Enhanced Primary Care | Group M03 | 10956 |
Focussed Psychological Strategies | Group M07 | 80125, 80126(T)(a), 80130, 80135, 80136(T)(a), 80140, 80145, 80146(T), 80150, 80151(T)(a), 80155, 80160, 80161(T)(a), 80165, 80170, 80171(T) | |
Group M17 | 91125(a), 91126(T)(a), 91130(a), 91135(a), 91136(T)(a), 91140(a), 91150(a), 91151(T)(a), 91155(a), 91160(a), 91161(T)(a), 91165(a) | ||
Group M18 (T) | 91172, 91173, 91185, 91186, 91175, 91176, 91187, 91188 | ||
Group M26 | 93356(a), 93357(T)(a), 93358(T)(a), 93359(a), 93360(T)(a), 93361(T)(a), 93362(a), 93363(T)(a), 93364(T)(a), 93365(a), 93366(T)(a), 93367(T)(a), 93326(a), 93327(a), 93322(a), 93323(a) | ||
Group M28 | 93385(a), 93386(a), 93383(a), 93384(a) | ||
Mental Health service | Group M11 | 81325 | |
Group M29 | 93506(a), 93529(a) | ||
Group M30 | 93551(a), 93584(a) | ||
Eating Disorder Treatment Service | Group M16 | 82350, 82351(T)(a), 82368, 82369(T)(a), 82370, 82371, 82372(T)(a), 82373, 82374, 82375(T), 82376, 82377(T)(a), 82378, 82379, 82380(T)(a), 82381, 82382, 82383(T) | |
Group M18 (T) | 93074, 93092, 93095, 93100, 93103, 93108, 93126, 93129, 93134, 93137 | ||
Paediatrician | Eating Disorder Treatment Plan preparation and review | Group A36 | 90261, 90263(T)(a), 90267, 90269(T)(a) |
Group A40 (T) | 92163, 92167(a), 92173, 92179(a) |
(a) Item discontinued
(T) Telehealth item
Provider type important notes
- General practitioner includes services provided by General practitioners and other medical practitioners, but excluding specialists or consultant physicians.
- Clinical psychologist includes item numbers that can only be claimed by eligible Clinical psychologists.
- Other psychologist includes item numbers that can be claimed by any eligible psychologist, clinical and other. The proportion of activity claimed against these items by Clinical psychologists has not been estimated in the presented data. That is, the services rendered by Clinical psychologists will be present in both the Clinical psychologist and Other psychologist categories.
Psychiatrist items – pre 1996
Restructuring of Group A8 items occurred as of 1 November 1996. Item numbers 134, 136, 138, 140, 142, 144, 146, 148, 150, 152, 153, 154, 155, 156, 157, 158 and 159 were discontinued as of 31 Oct 1996. Historical psychiatrist data includes services claimed against these item numbers.
Bushfire items
Item numbers for claims by people whose mental health was affected by a bushfire during 2019–20 and 2020–21 include services provided by:
- GPs: 894, 896, 898, 2121, 2150, 2196, 91283, 91285, 91286, 91287, 91371, 91372, 91721, 91723, 91725, 91727, 91729, 91731;
- Clinical psychologists: 91000, 91001, 91005, 91010, 91011, 91015;
- Other psychologists: 91100, 91101, 91105, 91110, 91111, 91115; and
- Other allied health: 91125, 91126, 91130, 91135, 91136, 91140, 91150, 91151, 91155, 91160, 91161, 91165.
Note, these items were discontinued on 30 June 2022.
BEACH Survey
The BEACH survey was conducted by the Family Medicine Research Centre at the University of Sydney from 1998 to 2016 and supported financially by government and private industry.
BEACH was the only continuous, randomised study of GP activity in the world and the only national program that provided direct linkage of all management actions to the problem. It provided information about GP encounters based on data collected from a sample of GPs. Data linkages between indication and patient management are unique to BEACH, where it was considered an important source for research into GP management of mental health services.
The number of estimated GP encounters deemed to be mental health related from the BEACH survey were greater than the number of Medicare-subsidised mental health specific services as not all mental health-related GP encounters were billed using mental health-specific MBS item numbers. The BEACH survey found the proportion of estimated GP mental health-related activity billed as Medicare-subsidised mental health specific GP services increased from around 11% in 2007–08 to around 18% in 2015–16. However, the cessation of the BEACH survey in 2016 prevents ongoing comparison between the BEACH survey data and the MBS data (Britt et al. 2016).
The AIHW is pursuing the identification of more recent alternative data sources to accurately present information on mental health care provided by GPs.
Additional information on the BEACH survey can be obtained from General practice activity in Australia 2015–16. Details on the data that were collected in the final 18th year of BEACH survey can be found in the archived reports and data section of Mental Health Online Report.
| Key concept | Description |
|---|---|
| Medicare-subsidised general practitioner (GP) services | Medicare-subsidised general practitioner (GP) services are services provided by medical practitioners who are vocationally registered under Section 3F of the Health Insurance Act 1973, or are Fellows of the Royal Australian College of General Practitioners or Fellows of the Australian College of Rural and Remote Medicine and meet the requirements for the relevant Quality Assurance and Continuing Medical Education program or trainees for vocational registration (DoH 2022: 21). GP mental health services include services provided by medical practitioners, including general practitioners, but excluding psychiatrists (DoH 2019: 107–166, 190, 218, 276–278, 456, 782, 1219–1223). |
| Medicare-subsidised other allied mental health services | Medicare-subsidised other allied mental health services are services provided by other allied mental health professionals such as occupational therapists, social workers and mental health nurses. These services cover focused psychological strategies – allied mental health (occupational therapist and social worker items) and enhanced primary care – allied health (mental health worker item). Mental health workers include Aboriginal health workers, mental health nurses, occupational therapists and some social workers as well as psychologists. Although some psychologists are covered by this item they cannot be readily separated from the other mental health workers covered, so this item is counted under the heading of other allied mental health services. The data source section lists these item groups and MBS item numbers. For Medicare payments to be made on these items the provider (occupational therapist, social worker or other appropriate provider) must be registered with Medicare Australia as meeting the credentialing requirements for provision of the service (DoH 2019: 1225–1231, 1294–1299, 1314–1315). |
| Medicare‑subsidised psychiatrist services | Medicare-subsidised psychiatrist services are services provided by a psychiatrist (or, for electroconvulsive therapy, by either a psychiatrist or another medical practitioner together with an anaesthetist) on a fee-for-service basis that are partially or fully funded under the Australian Government’s Medicare program. These services cover patient attendances (or consultations) provided in different settings as well as services such as group psychotherapy, telepsychiatry, case conferences and electroconvulsive therapy. These item groups along with the relevant MBS item numbers are listed in the data source section. Note that for items in the range 291 to 370 (MBS Group A8) and 855 to 866 (Case conference – consultant psychiatrist) only medical practitioners who are recognised as psychiatrists for the purposes of the Health Insurance Act 1973 are eligible to provide services attracting an MBS subsidy (DoH 2019: 69–72, 117–119, 227–237, 260–261, 323, 456). |
| Medicare-subsidised psychologist services | Medicare-subsidised psychologist services are services provided by psychologists that are rebatable by Medicare through psychological therapy services, focussed psychological strategies and enhanced primary care items. The data source section lists these item groups with the relevant MBS item numbers. For these items to be eligible for Medicare rebates, the provider must meet the following eligibility requirements and be registered with Medicare Australia. Medicare rebates for psychological therapy services are only available for services provided by clinical psychologists who are fully registered in the relevant jurisdiction and are members of, or eligible for membership with, the Australian Psychological Society’s College of Clinical Psychologists. Clinical membership is only available for registered psychologists who have completed the standard 4 years of study in psychology and attained an accredited doctorate degree in clinical psychology or master’s degree in clinical psychology with 1 year of supervised post-masters clinical psychology experience. Medicare rebates for focused psychological strategies and enhanced primary care are available for services provided by psychologists who are fully registered in the relevant jurisdiction regardless of any specialist clinical training. Registered psychologists must complete the standard 4 years of study in psychology with an additional 2 years of supervised practice, postgraduate coursework or a research degree, and meet any other jurisdiction-specific requirement for registration (DoH 2019: 77–78, 1219–1222, 1288–1291). |
| Psychologist (other) | Clinical psychologist includes psychological therapy services provided only by clinical psychologists. Psychologist (other) includes services provided by both clinical psychologists and other psychologists (DoH 2019: 77–78, 1286–1287, 1225–1231, 1239–1244, 1291–1294, 1305–1308, 1337). |
Britt H, Miller GC, Henderson J, Bayram C, Harrison C, Valenti L, Wong C, Gordon J, Pollack AJ, Pan Y and Charles J (2016) General practice activity in Australia 2015–16. General practice series no. 40, Sydney: Sydney University Press.
DoH (Department of Health) (2019) Medicare Benefits Schedule Book, effective 14 September 2019, Department of Health and Aged Care website, accessed 16 May 2022.
DoH (2020) Additional 10 MBS mental health sessions during COVID-19 under the Better Access Pandemic Support measure, Department of Health and Aged Care website, accessed 16 May 2022.
DoH (2022) Medicare Benefits Schedule Book, effective 16 May 2022, Department of Health and Aged Care website, accessed 16 May 2022.
Services Australia (2020) Information for allied health professionals. Better Access Initiative – supporting mental health care, Services Australia website, accessed 16 May 2022.
Data presented covers the time period 1984–85 to 2021–22. This section was last updated in April 2023.


