Diabetes-related complications
Page highlights:
- The most common diabetic complications present among adults living with diabetes attending services for diabetes care in 2021 were sexual dysfunction (12%), congestive cardiac failure (4.0%) and end-stage kidney disease (4.0%).
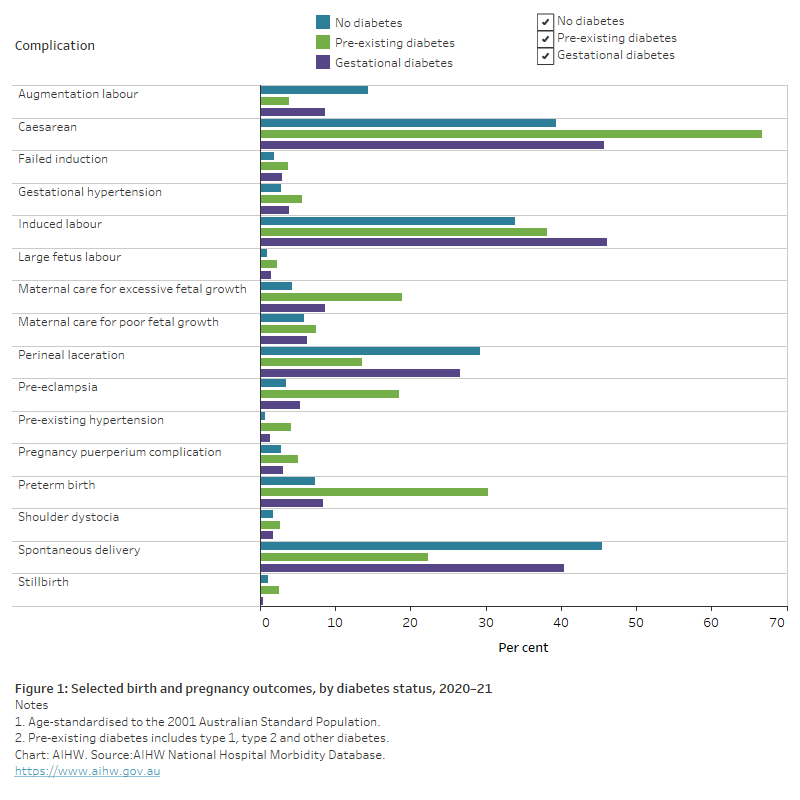
- In 2020–21, compared to mothers without diabetes, mothers living with pre-existing diabetes (and to a lesser extent, gestational diabetes), were more prone to complications during pregnancy and intervention in childbirth.
Diabetes-related complications are significant factors contributing to morbidity and mortality in Australia and are associated with increases in the costs associated with the treatment and management of diabetes (Lee et al. 2013; Twigg and Wong 2015). Diabetes is associated with both microvascular and macrovascular complications, especially in those with out-of-range diabetes management and higher long-term blood glucose levels (Stratton et al. 2000).
Diabetes complications may include:
- microvascular complications to the eye (retinopathy), kidney (nephropathy), and nerves (neuropathy)
- macrovascular complications affecting the circulatory system including ischemic heart disease, peripheral vascular disease and cerebrovascular disease
- an increased risk of other complications developing including foot ulcers (Reardon et al. 2020).
High blood glucose levels can also cause acute hyperglycaemic emergencies (Deed et al. 2018). These emergencies include:
- Ketoacidosis which is a life-threatening complication characterised by hyperglycaemia and high levels of blood acids (ketones) which is mostly found in people with type 1 diabetes.
- Hyperosmolarity which draws water from the body’s organs and is characterised by persistent hyperglycaemia without ketoacidosis, and is accompanied by profound dehydration.
Complications in primary care
The 2021 Australian Quality Clinical Audit 2021 Annual Report includes data collected for around 4,500 adults living with diabetes attending services for diabetes care. Many of these patients recorded complications related to diabetes.
In the last 12 months, the most common diabetic complications present in the cohort were:
- sexual dysfunction (12%)
- congestive cardiac failure (4.0%)
- end-stage kidney disease (4.0%)
- myocardial infarction (2.9%)
- coronary artery bypass graft (CABG)/angioplasty/stent (2.7%)
- blindness (1.9%)
- cerebral stroke (1.3%).
Prior to the last 12 months, the most common diabetic complications present in the cohort were:
- sexual dysfunction (12%)
- CABG/angioplasty/stent (10%)
- myocardial infarction (10%)
- cerebral stroke (5.0%)
- congestive cardiac failure (5.0%)
- end-stage kidney disease (5.0%)
- blindness (1.6%).
The most common foot complication reported in the cohort was peripheral neuropathy, which was recorded for 22% of patients in the last 12 months. Other diabetic foot complications in the last 12 months included foot ulceration (5.8%), peripheral vascular disease (7.6%) and lower limb amputation (1.7%).
Almost two-fifths of the cohort exhibited a form of proteinuria, either microalbuminuria (28%) or macroalbuminuria (10%) and more than a third of patients (33%) had chronic kidney disease (CKD). 56% of diabetes patients with CKD had middle-stage CKD (stage 3 or 4) (Australian National Diabetes Audit 2021).
Pregnancy complications
Diabetes in pregnancy, whether pre-existing (that is, type 1, type 2 or other diabetes type) or arising as a result of the pregnancy (gestational diabetes), is associated with an increased risk of adverse outcomes for the mother and child both during pregnancy, labour and delivery and in the longer term.
Note: The National Hospital Morbidity Database provides national data on pregnancies affected by diabetes, but International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification (ICD-10-AM) coding changes and the accuracy of recording diabetes type affect the ability to report on the number of pregnancies affected by and complications from pre-existing diabetes type. Further, in some cases, a definitive diagnosis of diabetes type cannot be made until after the birth of the baby, hence the initial diagnosis of gestational diabetes can include women with other forms of diabetes, detected for the first time in pregnancy (Nankervis et al. 2014).
Short-term outcomes
The complications and adverse outcomes experienced by mothers and their babies during pregnancy and delivery, vary between the types of diabetes (whether pre-existing or gestational diabetes), most likely due to the causes and effects of each diabetes type (AIHW 2019).
In 2020–21, compared to mothers without diabetes, mothers living with pre-existing diabetes (and to a lesser extent, gestational diabetes), were more prone to complications during pregnancy and intervention in childbirth. Having controlled for differences in the age structure of the populations, such complications include caesarean section, induced labour, maternal care for excessive fetal growth, pre-eclampsia and preterm birth (Figure 1).
Figure 1: Selected birth and pregnancy outcomes, by diabetes status, 2020–21
The horizontal bar chart shows selected birth and pregnancy outcomes for females by birth status in 2020–21. Compared to mothers without diabetes, mothers living with pre-existing diabetes (and to a lesser extent, gestational diabetes), were more prone to complications during pregnancy and childbirth such as caesarean section, induced labour, maternal care for excessive fetal growth, pre-eclampsia and preterm birth.
Longer-term outcomes
Diabetes in pregnancy is also associated with longer-term adverse outcomes for both mother and baby. For women diagnosed with gestational diabetes this includes an increased risk of recurrence of the condition in subsequent pregnancies with studies showing recurrence rates to vary between 30% and 84% (Kim et al. 2007). They also experience an increased risk for the development of type 2 diabetes, metabolic syndrome and cardiovascular disease.
Babies of mothers living with diabetes in pregnancy are also at an increased risk of childhood metabolic syndrome, obesity, impaired glucose tolerance and type 2 diabetes in later life (Clausen et al. 2007; Kim et al. 2012; Zhao et al. 2016).
Australian Institute of Health and Welfare (2019) Improving national reporting on diabetes in pregnancy: technical report, AIHW, Australian Government, accessed 10 March 2022.
Australian National Diabetes Audit (2021), Australian Quality Clinical Audit 2021 Annual Report, Department of Health, Australian Government, accessed 10 March 2022.
Clausen TD, Mathiesen ER, Hansen T, Pedersen O, Jensen DM, Lauenborg J et al. (2008), 'High prevalence of type 2 diabetes and pre-diabetes in adult offspring of women with gestational diabetes mellitus or type 1 diabetes—the role of intrauterine hyperglycaemia', Diabetes care, 31:340–46, doi:10.2337/dc07-1596.
Deed G, Manski-Nankervis JA, Barlow J, Zoungas S, Andrikopoulos S, Davis L et al. (2018) Emergency management of hyperglycaemia in primary care, The Royal Australian College of General Practitioners and Australian Diabetes Society joint clinical position statement, accessed 10 March 2022.
Kim C, Berger DK and Chamany S (2007), 'Recurrence of Gestational Diabetes Mellitus: a systematic review', Diabetes Care, 30(5):1314–1319, doi:10.2337/dc06-2517.
Kim SY, Sharma AJ and Callaghan WM (2012), 'Gestational diabetes and childhood obesity: what is the link?', Current Opinion in Obstetrics and Gynaecology, 24(6):376–81, doi:10.1097/GCO.0b013e328359f0f4.
Lee CM, Colagiuri R, Magliano DJ, Cameron AJ, Shaw J, Zimmet P, Colagiuri S (2013), 'The cost of diabetes in adults in Australia', Diabetes Research and Clinical Practice, 99(3): 385-90, doi:10.1016/j.diabres.2012.12.002.
Nankervis A, Mclntyre H, Moses R, Ross G, Callaway L, Porter C et al. (2014) ADIPS consensus guidelines for the testing and diagnosis of gestational diabetes mellitus in Australia, Sydney: Australasian Diabetes in Pregnancy Society.
Reardon R, Simring D, Kim B, Mortensen J, Williams D, and Leslie A (2020), 'The diabetic foot ulcer', Australian Journal of General Practice, 49(5): 250-255, doi:10.31128/AJGP-11-19-5161.
Stratton IM, Adler AI, Neil HAW, Matthews DR, Manley SE, Cull CA, et al. (2000), 'Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study', British Medical Journal, 321(7258): 405-412, doi:10.1136/bmj.321.7258.405.
Twigg SM and Wong J (2015), 'The imperative to prevent diabetes complications: a broadening spectrum and an increasing burden despite improved outcomes', The Medical Journal of Australia, 202(6): 300-4, doi:10.5694/mja14.01234.
Zhao P, Liu E, Qiao Y, Katzmarzyk PT, Chaput J-P, Fogelholm M et al. (2016), 'Maternal gestational diabetes and childhood obesity at age 9–11: results of a multinational study', Diabetologia, 59:2339–48, doi:10.1007/s00125-016-4062-9.


