Gestational diabetes
Page highlights:
- Testing for gestational diabetes is recommended for all pregnant women at 24–28 weeks gestation with re-testing at 6–12 weeks post-partum recommended for women diagnosed with gestational diabetes.
How common is gestational diabetes in Australia?
- More than 1 in 6 women (17.9%) who gave birth in 2021–22 was diagnosed with gestational diabetes (53,900 women).
Measuring diabetes in pregnancy
- Find out more about the data sources available for measuring diabetes in pregnancy.
Risk factors
The following factors (Nankervis et al. 2014) increase a woman’s risk of developing gestational diabetes:
- ethnicity: Asian, Indian subcontinent, Aboriginal, Torres Strait Islander, Pacific Islander, Māori, Middle Eastern, non-white African
- pre-pregnancy body mass index (BMI) >30 kg/m²
- previous hyperglycaemia in pregnancy
- previous elevated blood glucose level
- maternal age ≥40 years
- family history of diabetes mellitus (close relative with diabetes or a sister with hyperglycaemia in pregnancy)
- previous macrosomia (baby with birth weight >4500g or >90th percentile)
- polycystic ovary syndrome
- medications: corticosteroids, antipsychotics.
Diagnostic criteria
The Australasian Diabetes in Pregnancy Society guidelines recommend the 75g oral glucose tolerance test (OGTT) for all pregnant women at 24–28 weeks’ gestation and re-testing with the 75g OGTT at 6–12 weeks post-partum for women diagnosed with gestational diabetes. The post-partum test is to identify ongoing glucose issues which may indicate other forms of diabetes first detected in pregnancy. Regular, ongoing monitoring is also recommended due to the high risk of recurrence in subsequent pregnancies and of developing type 2 diabetes in the future.
A diagnosis for gestational diabetes (using the International Association of Diabetes and Pregnancy Study Groups criteria) is made based on the 75g OGTT with one or more of the following values (Nankervis et al. 2014):
- fasting plasma glucose ≥5.1mmol/L
- 1-hour post 75g oral glucose load ≥10.0 mmol/L
- 2-hour post 75g oral glucose load ≥8.5 mmol/L.
How common is gestational diabetes in Australia?
In 2021–22, more than 1 in 6 women (17.9%) aged 15–49 who gave birth in an Australian hospital were diagnosed with gestational diabetes (53,900 females), based on the National Hospital Morbidity Database.
Variation by age
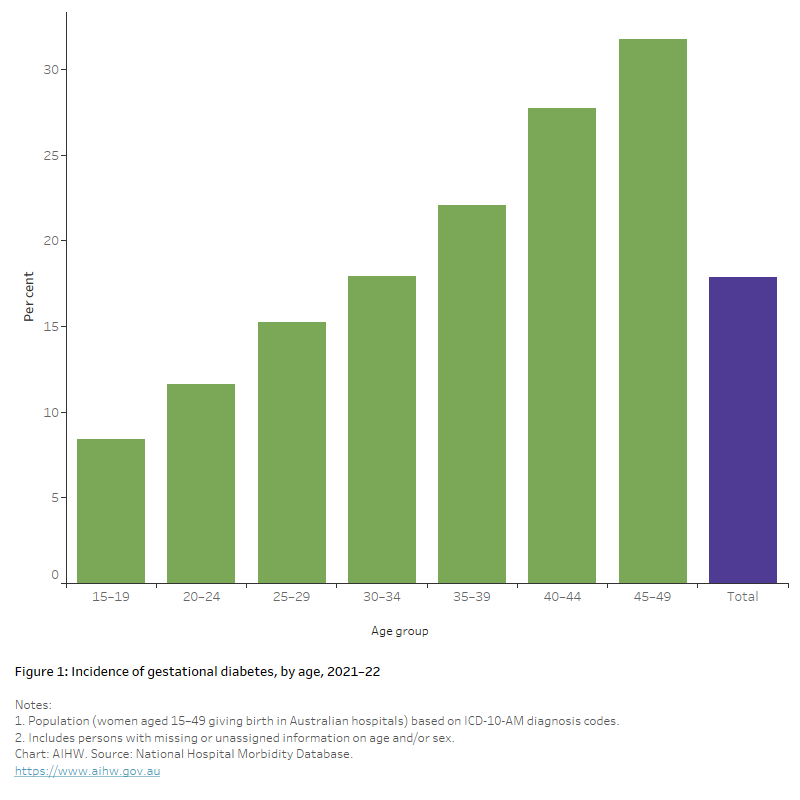
In 2021–22, the incidence of gestational diabetes increased with increasing maternal age, ranging from 8.4% to 31.7% in the 15–19 and 45–49 age groups, respectively. Compared with women aged 15–19, those aged 35–39 were 2.6 times as likely to be diagnosed with gestational diabetes while women aged 40–44 and 45–49 were 3.3 and 3.8 times as likely, respectively (Figure 1).
Figure 1: Incidence of gestational diabetes, by age, 2021–22
The chart shows the incidence of gestational diabetes by age group in 2021–22. Rates increased with increasing age, peaking in the 45–49 age group. Women in the 45–49 age group were 3.8 times as likely to be diagnosed with diabetes as women aged 15–19.
Trends over time
After adjusting for changes in the age structure of the population over time, the incidence of gestational diabetes more than doubled in Australia between 2012–13 and 2021–22. The most notable increases were recorded between 2012–13 and 2017–18 with a further upward spike in 2020–21 and 2021–22 (Figure 2).
Note: The rising incidence of gestational diabetes in the last decade is likely driven by several factors including increasing maternal age, higher rates of maternal overweight and obesity, and a growing proportion of higher risk ethnic groups in the population (Laurie and McIntyre 2020). The introduction of new diagnostic guidelines across all states and territories between 2011 and 2013 and the establishment of the National Gestational Diabetes Register (NGDR) in 2011 may also have had an impact on rates. Refer to Incidence of gestational diabetes in Australia – Changing trends for further information.
Figure 2: Incidence of gestational diabetes, 2011–12 to 2021–22
The chart shows the proportion of females diagnosed with gestational diabetes in Australia more than doubled from 9.3% in 2012–13 to 19.3% in 2021–22. Caution should be taken when comparing rates over time as many factors, including new diagnostic guidelines, are likely to have had an impact on the number of females diagnosed with gestational diabetes in recent years.

Variation between population groups
Aboriginal and Torres Strait Islander women
In 2020–21:
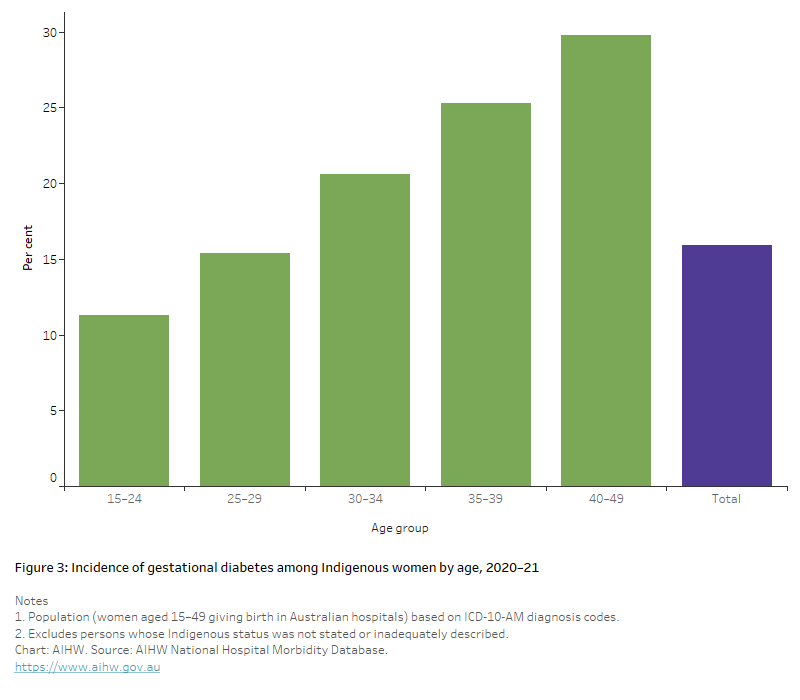
- there were around 2,400 new cases of gestational diabetes among Aboriginal and Torres Strait Islander women, equating to 16% of Indigenous women who gave birth in hospital.
- the incidence of gestational diabetes increased with increasing age, peaking in the 40–49 age group at 30% which is about 2.6 times that of those aged 15–24 (11.3%) (Figure 3).
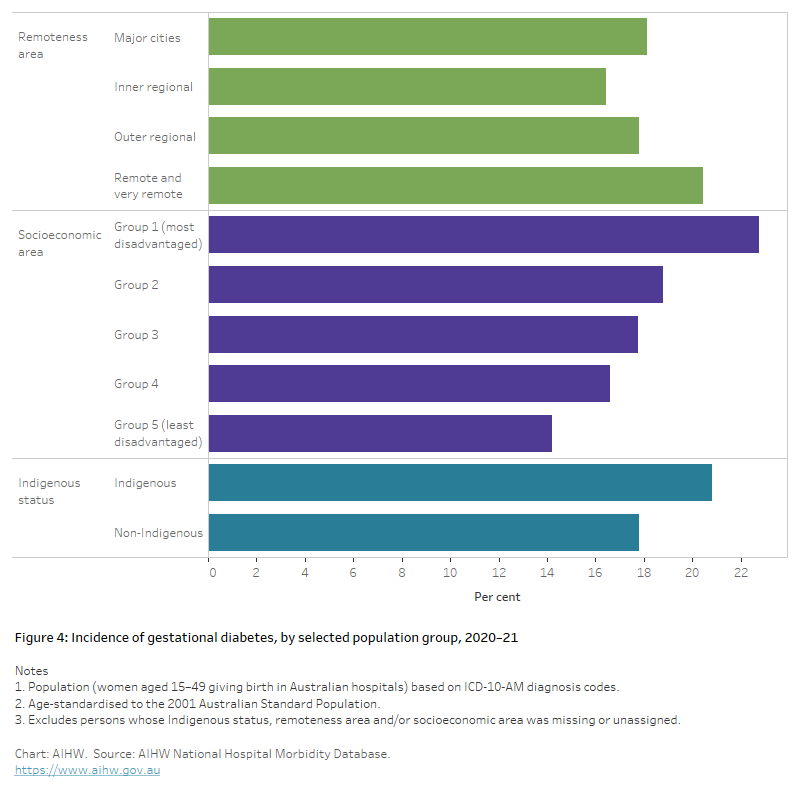
- After adjusting for differences in the age structure of the populations, Indigenous women were 1.2 times as likely to be diagnosed with gestational diabetes as non-Indigenous women (Figure 4).
Figure 3: Incidence of gestational diabetes among Indigenous women by age, 2020–21
The chart shows the incidence of gestational diabetes among Indigenous women by age group in 2020–21. Rates increased with increasing age, peaking in the 40–49 age group. Women in the 40–44 age group were 2.6 times more likely to be diagnosed with diabetes than those aged 15–24.
Remoteness area
In 2020–21, the incidence of gestational diabetes was slightly higher among those living in Remote and very remote areas (1.1 and 1.2 times as high as those living in Major cities and Inner regional areas, respectively) (Figure 4).
Socioeconomic area
In 2020–21, the incidence of gestational diabetes increased with increasing levels of socioeconomic disadvantage. After adjusting for differences in the age structure of the populations, women living in the lowest socioeconomic areas were 1.6 times as likely to be diagnosed with gestational diabetes as those living in the highest socioeconomic areas (Figure 4).
Figure 4: Incidence of gestational diabetes, by selected population groups, 2020–21
The chart shows the incidence of gestational diabetes by selected population groups in 2020–21. Incidence rates increased with increasing socioeconomic disadvantage with women living in the most disadvantaged areas being 1.6 times as likely to be diagnosed with gestational diabetes as those living in the least disadvantaged areas. Incidence rates were slightly higher among those living in Remote and very remote areas.
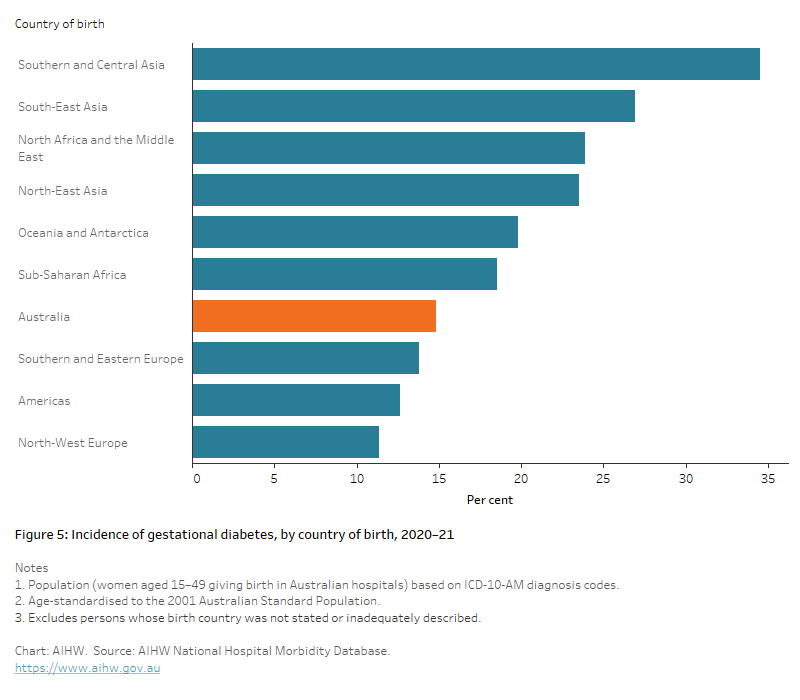
Country of birth
In 2020–21, after adjusting for differences in the age structure of the populations, compared with women born in Australia:
- women born in Southern and Central Asia, South–east Asia, North Africa and the Middle East and North–East Asia were between 1.6 and 2.3 times as likely to be diagnosed with gestational diabetes
- women born in North–West Europe and the Americas were slightly less likely (0.8 and 0.9 times) to be diagnosed with gestational diabetes, respectively (Figure 5).
Figure 5: Incidence of gestational diabetes, by country of birth, 2020–21
The chart shows the age-standardised incidence of gestational diabetes by country of birth in 2020–21. Compared with women born in Australia, those born in Southern and Central Asia and South-East Asia were 2.3 and 1.6 times as likely to be diagnosed with gestational diabetes while women born in the Americas and North-West Europe were both 0.8 and 0.9 times as likely, respectively.
Measuring diabetes in pregnancy
Measuring the number of women living with gestational diabetes or pre-existing diabetes during pregnancy at a given time (prevalence) is not as useful as measuring the total number of diabetes-impacted pregnancies (incidence).
The 3 primary sources of data available to report on diabetes in pregnancy at the national level are:
- National Perinatal Data Collection (NPDC)
- National Hospital Morbidity Database (NHMD)
- National Diabetes Services Scheme (NDSS).
These data sources are administrative data sets designed to collect information primarily for administrative purposes, so might not always be suitable for monitoring complex health issues and research.
National Hospital Morbidity Database (NHMD)
In this report, the NHMD is the primary data source used to report gestational diabetes incidence and complications associated with both gestational diabetes and pre-existing diabetes in pregnancy. The NHMD contains episode-level records from admitted patient data collection systems in Australian public and private hospitals and includes administrative, demographic and clinical data. The NHMD captures virtually all births in Australia, with 97% of babies born in a hospital (AIHW 2021) and allows the calculation of a national estimate of gestational diabetes incidence. The NHMD provides national data on pregnancies affected by diabetes, and some complications and interventions. Data from the NHMD enable new cases of gestational diabetes in Australia over time to be identified. While the NHMD allows for the differentiation between pre-existing diabetes types using ICD-10-AM codes, changes to the ICD-10-AM coding, and the accuracy of recording diabetes type have an impact on the ability to report complications by diabetes type from the NHMD (AIHW 2014; Knight et al. 2011).
National Perinatal Data Collection (NPDC)
Compared with the other data sources (NHMD and NDSS), the NPDC provides comprehensive data for assessing the short-term impact of diabetes in pregnancy on the health of mothers and babies. But national data for all pregnancies affected by diabetes are not available for reporting, as data on diabetes status in Victoria are not currently collected in a format comparable with the specifications for the NPDC, so are excluded when reporting on the impact of diabetes in pregnancy. Data are also not currently of sufficient quality to assess diabetes type at the national level, as some jurisdictions are unable to distinguish between pre-existing diabetes types. Before 2014, information for diabetes type was provided, but varied across jurisdictions, so data cannot be compared with data collected after 2014.
National Diabetes Services Scheme (NDSS)
The NDSS allows the number of women with gestational diabetes to be identified at the national level, including the number of women having a repeat diagnosis of gestational diabetes, and provides information about the number of women who are using insulin therapy as the method of treatment for their condition. But the NDSS cannot be used to assess pre-existing diabetes in pregnancy or be used to assess pregnancy-related complications or outcomes.
Note: A definitive diagnosis of gestational diabetes cannot be made until after the birth of the baby, hence the initial diagnosis of gestational diabetes can include women with other forms of diabetes, detected for the first time in pregnancy (Nankervis et al. 2014).
AIHW (Australian Institute of Health and Welfare) (2014) Cardiovascular disease, diabetes and chronic kidney disease—Australian facts: morbidity—hospital care, AIHW, Australian Government, accessed 1 December 2021.
AIHW (2019) Incidence of gestational diabetes in Australia, AIHW, Australian Government, accessed 19 August 2022.
AIHW (2021) Australia's mothers and babies, AIHW, Australian Government, accessed 08 September 2021.
Knight KM, Thornburg LL and Pressman EK (2012), 'Pregnancy outcomes in type 2 diabetic patients as compared with type 1 diabetic patients and nondiabetic controls', The Journal of Reproductive Medicine, 57(9–10):397–404, PMID: 23091986.
Laurie J and McIntyre D (2020) ‘A Review of the Current Status of Gestational Diabetes Mellitus in Australia–The Clinical Impact of Changing Population Demographics and Diagnostic Criteria on Prevalence’, International Journal of Environmental Research and Public Health, 17(24):9387, doi:10.3390/ijerph17249387.
Nankervis A, Mclntyre H, Moses R, Ross G, Callaway L, Porter C et al. (2014) ADIPS consensus guidelines for the testing and diagnosis of gestational diabetes mellitus in Australia. Sydney: Australasian Diabetes in Pregnancy Society.


