Health system expenditure
Page highlights:
How much is spent on diabetes?
- In 2020–21, an estimated $3.4 billion of expenditure in the Australian health system was attributed to diabetes, representing 2.3% of total disease expenditure.
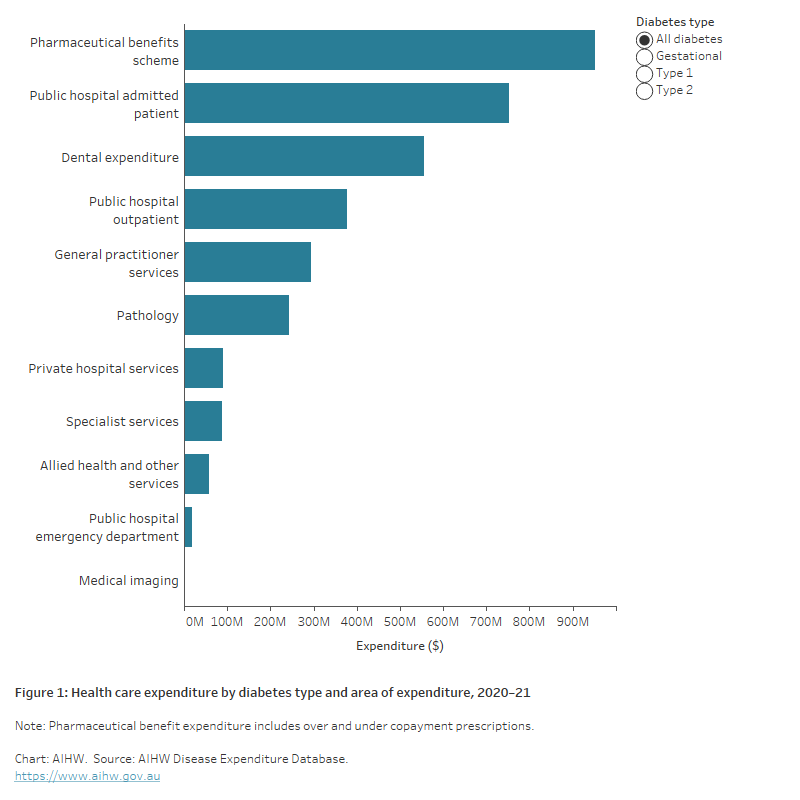
- Medications dispensed through the Pharmaceutical Benefits Scheme accounted for 28% of total diabetes expenditure and was the single highest area of health system spending with $952.7 million.
- The combined spending on hospital services accounted for 36% ($1.2 billion).
What is health system expenditure on diabetes?
This section provides recent data on health system expenditure on diabetes, with details by diabetes type, health-care service, age group, and sex. It includes expenditure by the Australian Government, state, territory and local governments and the non-government sector (including private health insurance and individual contributions). These estimates report direct, allocated and recurrent expenditure only. They do not account for the total amount spent on diabetes health.
Further information on how the estimates were derived is available from Health system spending on disease and injury in Australia 2020–21.
How much is spent on diabetes?
Of the $3.4 billion health system expenditure attributed to diabetes in 2020–21, an estimated:
- $373 million was attributed to type 1 diabetes
- $2.3 billion was attributed to type 2 diabetes
- $71.6 million was attributed to gestational diabetes
- $668.2 million was attributed to ‘other/unspecified’ diabetes (AIHW 2023).
Note: Due to the high number of ‘other/unspecified’ diabetes, caution should be used when interpreting data by diabetes type.
Where is the money spent?
In 2020–21, medications dispensed through the Pharmaceutical Benefits Scheme (PBS) was the single highest area of health system spending for diabetes accounting for 28% of total diabetes expenditure ($952.7 million). The combined spending on hospital services accounted for 36% (1.2 billion). This included expenditure on public hospital admitted patients ($752.2 million), public hospital outpatients ($376.7 million), private hospital services ($89.6 million), and public hospital emergency departments ($18.9 million) (Figure 1).
Figure 1: Health care expenditure on diabetes, by area of expenditure, 2020–21
The chart shows health care expenditure on diabetes by type and area of expenditure in 2020–21. For all diabetes, type 1 and type 2 diabetes medications dispensed through the Pharmaceutical Benefits Scheme was the highest area of expenditure followed by public hospital admitted patients.
Who is the money spent on?
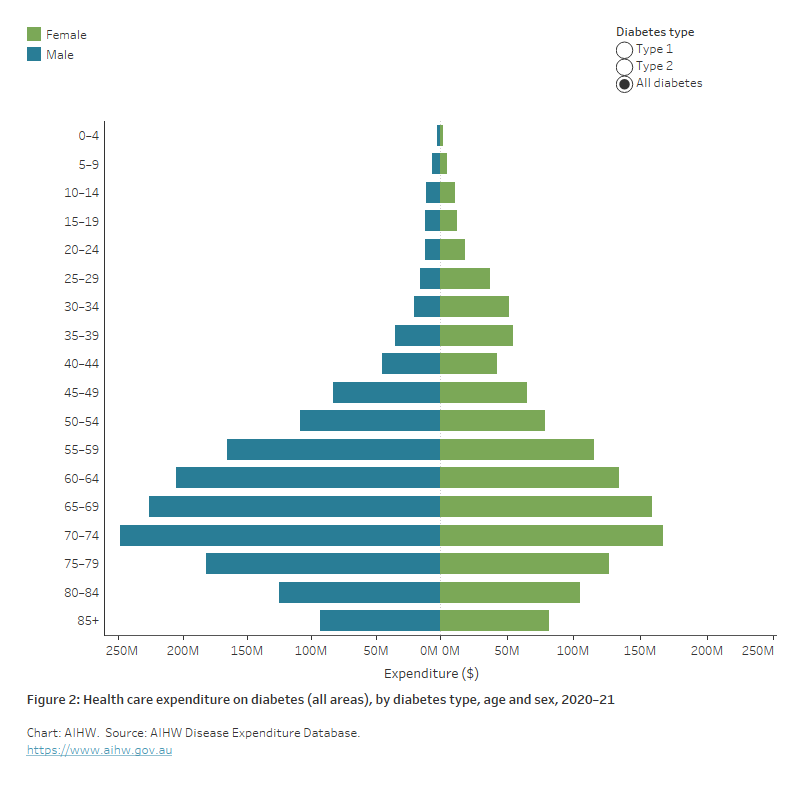
The health system expenditure attributed to all diabetes varies significantly according to age and sex.
In 2020–21:
- total disease expenditure was about 1.3 times as high in males compared with females ($1.6 billion and $1.3 billion, respectively).
- total diabetes expenditure generally increased with increasing age with around 63% being spent on people aged 55 and over and peaking in the 70–74 age group at $422.9 million. A similar pattern of expenditure is seen for males and females, separately (Figure 2).
Figure 2: Health care expenditure on diabetes (all areas), by diabetes type, age and sex, 2020–21
The chart shows the overall health system expenditure on diabetes by 5-year age group and sex in 2020–21 by diabetes type. Expenditure peaked in the 70–74 age group for all diabetes types yet was more pronounced in the younger age groups for type 1 diabetes than type 2 diabetes.
Aboriginal and Torres Strait Islander People
In 2015–16, expenditure on potentially preventable hospitalisations (PPH) was 2.2 times as high in Aboriginal and Torres Strait Islander people compared with non-Indigenous Australians ($392 and $176, respectively). Notably, the greatest difference in expenditure is attributed to diabetes, a gap of $33 per person (AIHW and NIAA 2020).
References
Australian Institute of Health and Welfare (2023) Health system spending on disease and injury in Australia 2020–21, AIHW, Australian Government, accessed 30 November 2023.
AIHW and NIAA (National Indigenous Australians Agency) (2020) 3.21 Expenditure on Aboriginal and Torres Strait Islander health compared to need - AIHW Indigenous HPF, AIHW and NIAA, Australian Government, accessed 24 March 2022.


