Behaviours captured in aged care assessments
To access government-subsidised aged care services, a person will undertake an initial screening to establish their needs and the types of services that could help them. Only the most comprehensive type of assessment captures behaviour and psychological symptoms. For more information on aged care assessments, please visit Aged care assessments.
Behaviours recorded in comprehensive aged care assessments compared to the Neuropsychiatric Inventory (NPI)
As discussed in the previous section, the NPI is the gold-standard assessment for identifying BPSD. However, the NPI is not undertaken for people accessing government funded aged care services. Instead, select behaviours are recorded in comprehensive aged care assessments that align with descriptions of some BPSD domains in the NPI.
While the information presented below provide useful insight on the symptoms experienced by people accessing aged care services, ‘symptoms’ recorded in a comprehensive aged care assessment do not reflect the preferred clinical terms. For example, the description of NPI domain disinhibition overlaps with the recorded symptom, risky behaviours, in a comprehensive aged care assessment. While we present information on people experiencing risky behaviours below as recorded in the comprehensive aged care assessment data, disinhibition remains the preferred clinical term. Further, while wandering is not listed in the NPI, it is frequently cited as an example of BPSD in literature (RACGP 2019; Burley et al. 2021) and is listed as an example behaviour under the Sleep and Nighttime Behaviours NPI domain. As such, wandering information collected in the comprehensive assessments have been included in this section.
In 2021–22, nearly 199,400 Australians completed a comprehensive aged care assessment and 16% (32,600) of people were recorded as having dementia. Among all people who completed a comprehensive aged care assessment, 41% reported experiencing one or more behaviours or psychological symptoms ‘regularly’ or ‘always.’
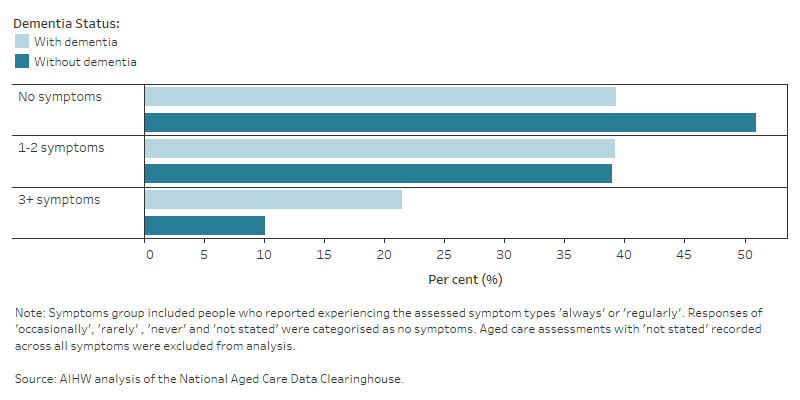
A higher proportion of people with dementia reported experiencing one or more symptoms compared with people without dementia (61% compared with 49%, respectively). In addition, the proportion of people with dementia who reported experiencing three or more symptoms always or regularly was more than twice as high as the proportion of people without dementia (22% compared with 10%, respectively) (Figure 15.2).
- Agitation – described as extreme emotional disturbance.
- Anxiety – described as an unpleasant state of inner turmoil, often accompanied by nervous behaviours such as pacing back and forth, somatic complaints and rumination.
- Apathy – described as the absence or suppression of passion, emotion, or excitement.
- Depression – described as depressive symptoms, including physical symptoms, long periods of feeling lonely, overwhelming feelings of being unable to keep going or regular tears.
- Hallucinations or delusions – delusions are described as false or erroneous beliefs that usually involve a misinterpretation of perceptions or experiences. Hallucinations can occur in any sensory modality, including auditory, visual, olfactory (smell), gustatory (taste) and tactile (touch).
- Insomnia – described as persistent difficulty in initiating or maintaining sleep.
- Risky behaviour – described as behaviours that put the person or others at risk of harm.
- Resistive behaviour – described as a person resisting, opposing or withstanding help or caregiving tasks such as taking medication, eating or self-feeding.
- Verbal aggression – described as a person yelling, screaming and/or threatening.
- Wandering – described as moving without definite destination or purpose.
Figure 15.2: Proportion of people who completed a comprehensive aged care assessment in 2021–22, by number of behaviours and psychological symptoms and dementia status
Horizontal bar graph showing that a greater proportion of people without dementia recorded zero symptoms, while a greater proportion of people with dementia recorded three or more symptoms.
Symptom types
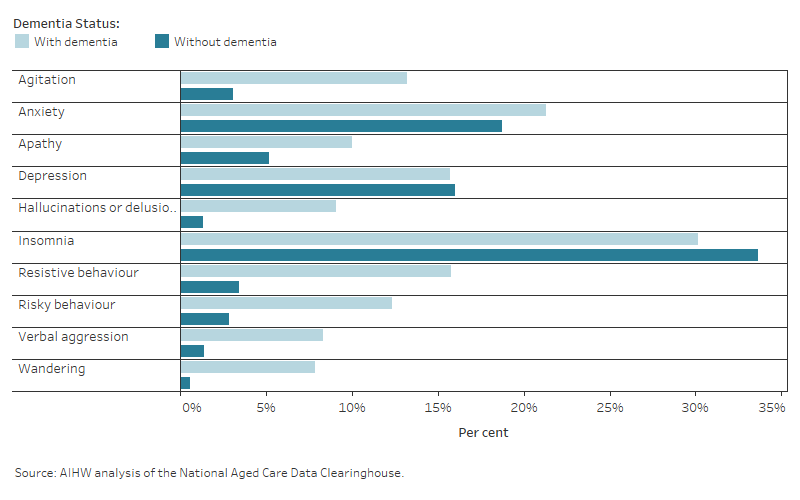
Insomnia was the most frequently reported symptom among people who completed a comprehensive aged care assessment in 2021–22 and rates were similar among people with dementia and people without dementia (30% and 34%, respectively). This was followed by anxiety (21% and 19%, respectively) and resistive behaviours (16% and 3.4%, respectively).
When comparing symptom frequency by dementia status, the following symptoms had the greatest percentage point difference:
- Resistive behaviours – (16% of people with dementia compared with 3.4% of people without dementia).
- Agitation – (13% of people with dementia compared with 3.1% of people without dementia).
- Risky behaviours – (12% of people with dementia compared with 2.9% of people without dementia) (Figure 15.3a).
It is important to note that while frequency of symptoms is captured within the comprehensive aged care assessment data, there is no indication of symptom severity or carer distress. Data in this section are based on an individual reporting their experience of a particular symptom to be ‘always’ or ‘regularly,’ however it is difficult to estimate the full extent of symptom impact without further severity and distress information.
Figure 15.3a: Proportion of people who reported experiencing behaviours and psychological symptoms ‘always’ or ‘regularly’ in comprehensive aged care assessment in 2021–22, by symptom type
Horizontal bar graph showing that insomnia was the most recorded symptom among people with and without dementia.
Symptoms decreased with age and varied by sex
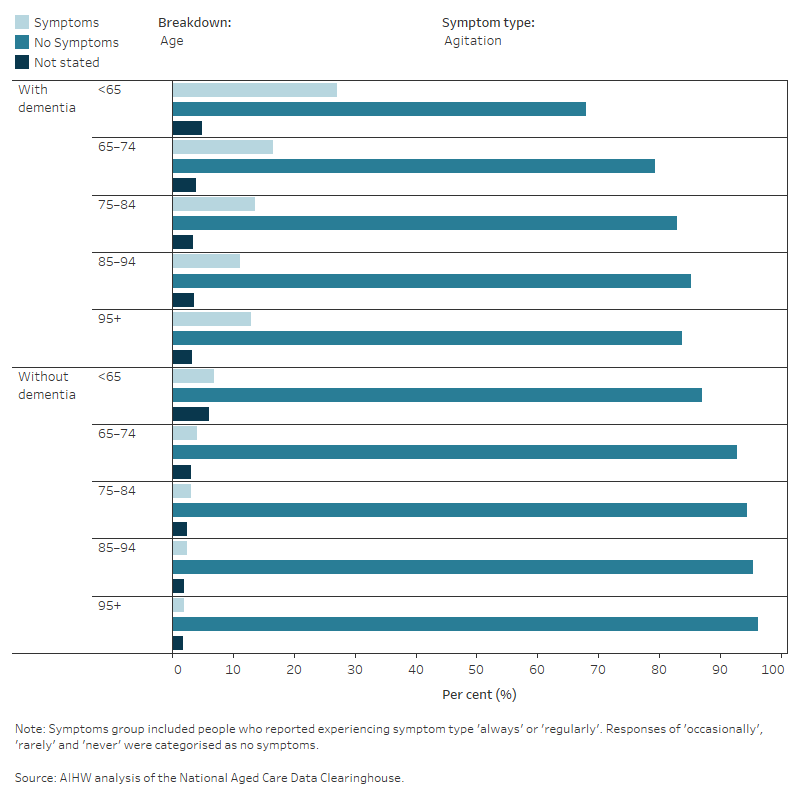
Among people who completed a comprehensive aged care assessment and had dementia recorded as a health condition:
- A higher proportion of men reported experiencing symptoms of agitation, apathy, insomnia, risky behaviour, verbal aggression and wandering ‘always’ or ‘regularly’ compared with women. A higher proportion of women reported experiencing symptoms of anxiety, depression and resistive behaviours ‘always’ or ‘regularly’ compared with men.
- Symptoms of resistive behaviour, agitation, apathy and insomnia decreased with age until ages 85–94, followed by a slight increase in the 95+ age group. Symptoms of hallucinations or delusions varied over the age groups. Across all remaining symptom types, rates decreased with age, except for depression, which increased in the 65–74 age group and then decreased (Figure 15.3b).
Within Figure 15.3b, the proportion of the ‘not stated’ responses are presented for each symptom. Across all symptom types, there were a greater proportion of ‘not stated’ responses for people who recorded dementia as a health condition compared to people who did not. As such, it is likely that these estimates disproportionately undercount the frequency of symptoms experienced among people with dementia who completed a comprehensive aged care assessment.
Figure 15.3b: Reported symptoms among people who completed a comprehensive aged care assessment in 2021–22, by symptom type, age and sex
Horizontal bar graph showing that reported symptoms from people with or without dementia decreased with age. Overall, except for insomnia and depression, people with dementia were more likely to report symptoms than people without dementia.
Triggers for assessment
Comprehensive aged care assessments record the triggers that indicate the need for an individual’s assessment to take place. These triggers may be closely related to an individual’s health and care needs, or related to other circumstances such as a change in care arrangements. An individual may also have more than one trigger for assessment recorded.
Comprehensive aged care assessments for people with dementia who reported behaviours or psychological symptoms were most commonly triggered by a change in cognitive status (85%), change in care needs (79%), and change in medical condition (74%). These triggers were similarly common among people with dementia who did not report symptoms (79%, 75% and 72% respectively). Across every trigger, there was a higher proportion of people with symptoms recorded compared with people without symptoms (Table S15.10).
Burley C, Casey AN, Chenoweth L and Brodaty H (2021) ‘Reconceptualising Behavioural and Psychological Symptoms of Dementia: Views of People Living With Dementia and Families/Care Partners’, Frontiers in Psychiatry, doi: doi.org/10.3389/fpsyt.2021.710703.
RACGP (Royal Australian College of General Practitioner) (2019) RACGP aged care clinical guide (Silver Book), RACGP, accessed 11 November 2022.


