Deaths due to dementia
Key statistics




Dementia is a progressive condition that leads to reduced life expectancy. However, time from diagnosis to death is highly variable. Survival time is affected by age, sex, dementia type and severity at diagnosis, among other factors (Brodaty et al. 2012). In addition, dementia is not always the direct cause of death as the condition often impairs an individual’s physical health and their ability to cope with other diseases (Dementia Australia 2019).
The mortality statistics presented here are derived from the National Mortality Database and, unless otherwise specified, refer to cases where a death was due to dementia, also known as the ‘underlying cause of death’. The National Mortality Database holds records for deaths in Australia from 1964 and comprises information about causes of death and other characteristics of the person, such as sex, age at death, area of usual residence and First Nations status. Causes of death were coded using the 10th version of the International Statistical Classification of Diseases and Related Health Problems (ICD-10), an international standard agreed by the World Health Organization for defining and reporting causes of death. Refer to the Technical notes for further information on death data and the codes used to classify dementia in the National Mortality Database.
Refer to the Mortality data tables for underlying data presented in these pages.
Dementia is a leading cause of death in Australia
In 2021, dementia was the second leading cause of death in Australia after coronary heart disease, and was the leading cause of death for women. There were a total of 15,800 deaths due to dementia, with more women than men dying due to the condition (around 10,100 and just over 5,700 deaths, respectively). This corresponds to dementia causing 10% of all deaths in Australia in 2021 (or 13.1% of all deaths among women and 6.9% of all deaths among men).
Figure 3.1 shows the leading 5 causes of death for Australians in 2021, by age and sex. Dementia becomes an increasingly common cause of death with increasing age, and was the leading cause of death for persons aged 75 and over. This was driven by the fact that dementia was the leading cause of death for women aged 75 and over. For men aged 75 and over, dementia was the second leading cause of death after coronary heart disease.
Details on the total number of deaths and the age-specific rate of deaths per 100,000 population are displayed when the mouse is hovered over each leading cause of death.
Figure 3.1: Leading causes of death in Australia in 2021, by age and sex
Figure 3.1 shows that dementia becomes an increasingly common cause of death with increasing age, and was the leading cause of death for persons aged 75 and over.
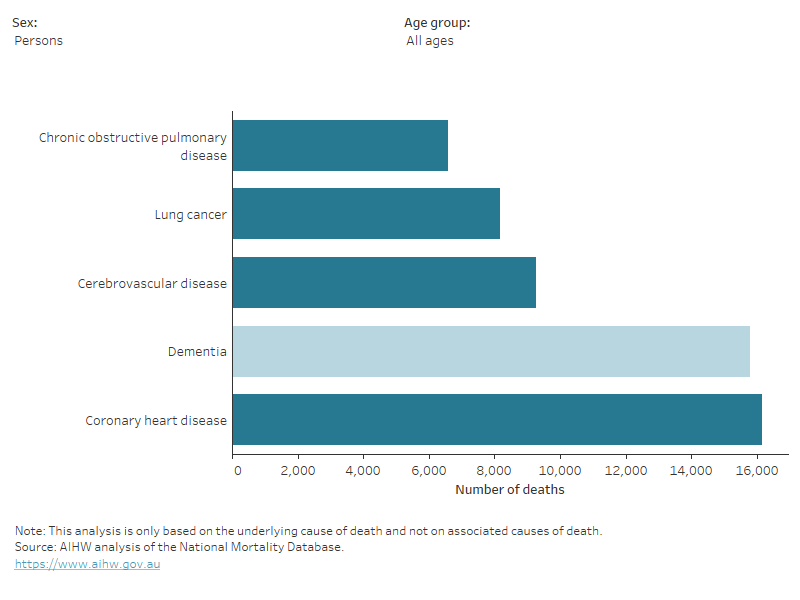
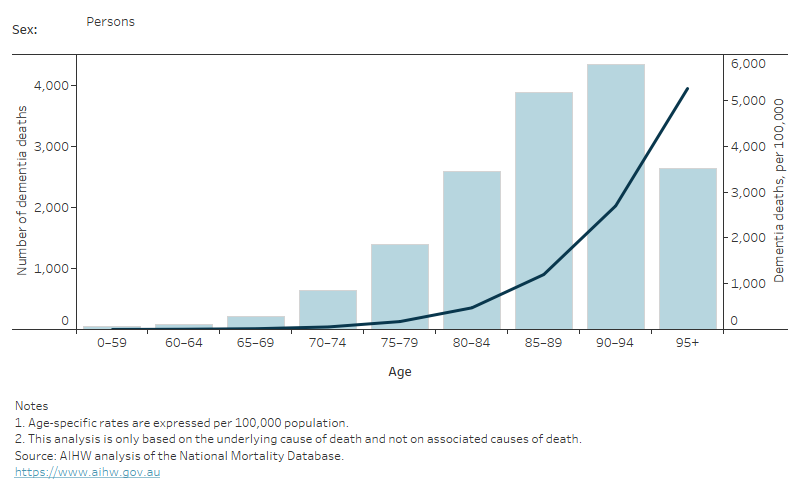
Figure 3.2 presents more details on deaths due to dementia by age and sex in 2021. The rate of deaths due to dementia among those who died aged 75–79 was 175 and 171 deaths per 100,000 population for men and women, respectively. The rate increased to just over 4,000 and 5,700 per 100,000 population for men and women aged 95 and over, respectively. The majority of deaths due to dementia occurred among men and women aged 85–94 years.
Figure 3.2: Deaths due to dementia in 2021: number and age-specific rates, by age and sex
This figure shows the increasing number and rate of deaths due to dementia, with most deaths occurring among people aged between 85 and 94.
Box 3.1: Provisional dementia deaths in more recent years
The current Dementia in Australia report includes mortality data up to and including 2021. This data includes the latest available coroner and doctor certified deaths data which are compiled and provided to the AIHW by the ABS. In response to the COVID-19 pandemic, the ABS started reporting provisional mortality statistics.
The latest provisional mortality estimates indicate an upward trend in deaths due to dementia. Over the year to date in 2023, deaths due to dementia were above the baseline average in the years of 2017–2019, and in 2021, and above the number of deaths recorded at a similar point in 2022 (ABS 2023).
Provisional mortality data includes deaths certified by doctors only and does not include deaths referred to the coroner (around 15% of total deaths). Therefore, data released provisionally is subject to change and should be interpreted with caution. However it does provide an early indication of emerging mortality patterns in Australia.
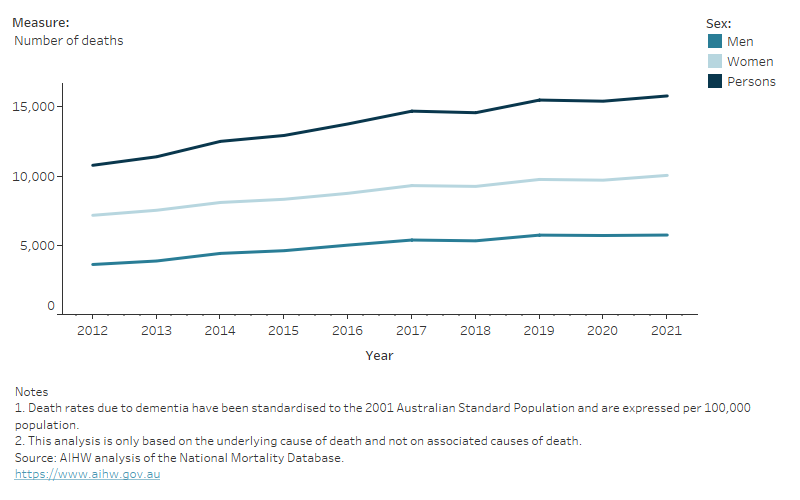
Deaths due to dementia have increased over the 2012–2021 period
The number of deaths due to dementia increased from 10,800 deaths in 2012 to 15,800 deaths in 2021 (Figure 3.3). This increase was seen for both men and women. Each year more women than men died due to dementia. As age is the biggest risk factor for dementia, the increase in the number of Australians dying from dementia is in part a reflection of more Australians living to older ages.
The rate of deaths due to dementia increased from 47 to 61 deaths per 100,000 population between 2012 and 2021 (Table S3.3). However, a large part of this increase was due to Australia’s increasingly ageing population. When accounting for changes in the Australian population over time, the age-standardised rate of deaths due to dementia between 2012 and 2021 increased slightly from 38 to 41 deaths per 100,000 population.
Over the period 2012 to 2021, age-standardised death rates increased slightly for both men (from 34 to 37 deaths per 100,000) and women (from 39 to 43 deaths per 100,000). The increase in the number of deaths due to dementia may not be entirely explained by Australia’s increasingly ageing population, and the prevalence of dementia may have also changed over the period from 2012 to 2021.
Other factors that may have contributed to changes in the number and rate of deaths due to dementia over the last decade include:
- Changes in ICD-10 instructions for coding deaths data have resulted in the assignment of some deaths to Vascular dementia (F01) where previously they may have been coded to Cerebrovascular diseases (I60–I69).
- Legal changes allowing veterans and members of the defence forces to relate death from vascular dementia to relevant service and an accompanying promotional campaign targeted at health professionals, are thought to have increased the number of dementia deaths among this group (ABS 2015).
Figure 3.3: Deaths due to dementia in Australia over the period 2012 to 2021: number and age-standardised rate by sex
This figure shows the number and age-standardised rates of men, women and people who died due to dementia in Australia between 2012 and 2021.
How are dementia types coded in death certificates?
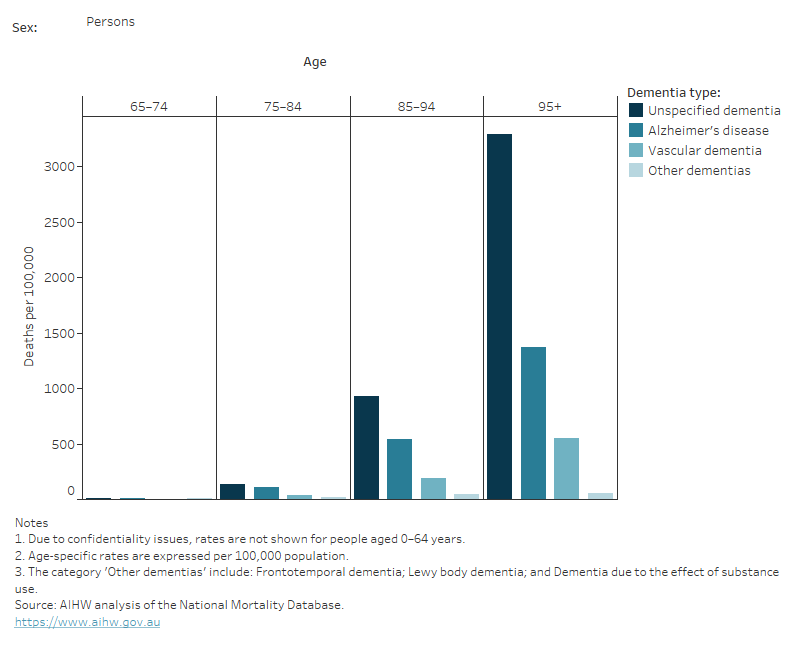
Although the National Mortality Database contains information on specific types of dementia, this information is not always systematically recorded on death certificates. Coding changes and variations in certification practices have likely resulted in an increase in deaths coded to dementia (ABS 2015). Descriptions in death certificates may indicate dementia but not a particular type of dementia, and in these cases, the type of dementia would be recorded as Unspecified dementia. These influencing factors should be kept in mind when interpreting deaths by dementia type.
In 2021, for people aged 65 and over, the most common specific dementia types recorded were Alzheimer’s disease (just over 5,000 deaths) and Vascular dementia (1,700 deaths). Unspecified dementia, that is, when the type of dementia was not known, was recorded for 8,300 deaths (Table S3.4). Together, Frontotemporal dementia, Lewy body dementia and Dementia due to the effects of substance use, accounted for 660 deaths. Interestingly, as age increased, so did the age-specific rate of deaths classified as due to Unspecified dementia (Figure 3.4). This may be due to challenges in diagnosing and reporting dementia among older individuals who have other comorbidities, and similar trends have been found in other recent studies (Gao et al. 2018; PHE 2016).
Figure 3.4: Deaths due to dementia in 2021: age-specific rates, by sex and dementia type
This figure shows that Unspecified dementia was responsible for the highest rate of deaths, followed by Alzheimer’s disease and Vascular dementia.
Emerging work in Australia to better understand dementia typing in deaths data
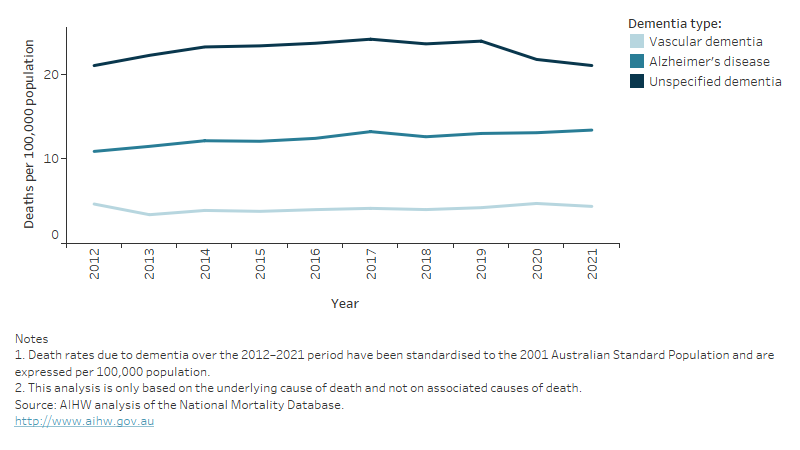
Over the 2012–2021 period, the age-standardised rate of deaths due to Unspecified dementia increased from 21 to 24 deaths per 100,000 people between 2012 and 2016, then remained steady before decreasing to 22 deaths per 100,000 people in 2020. The age-standardised rate of deaths decreased again in 2021 to 21 deaths per 100,000 people (Figure 3.5). Crude rates of deaths per 100,000 due to Unspecified dementia followed a similar trend (Table S3.5). The reasons for this trend are not well understood.
The Australian Bureau of Statistics (ABS) and the University of Queensland are currently analysing changes in how dementia deaths have been certified by doctors over time. This analysis will also examine the interaction between certified terms and the application of ICD mortality coding rules as well as differences across jurisdictions. This work will be valuable to understand what is driving changes in dementia typing over time and how data users should interpret coding changes over time, and may lead to recommendations that could improve the specificity of dementia types in future data sets. Recommendations will also be provided to certifiers on how recording of dementia deaths can be improved (NHMRC 2019).
Figure 3.5: Deaths due to dementia over the period 2012 to 2021: age-standardised rates, by dementia type
This figure shows the age-standardised rates of deaths due to dementia in Australia between 2012 and 2021 by type of dementia (Alzheimer’s disease, Unspecified dementia, Vascular dementia).
Geographic and socioeconomic area variations
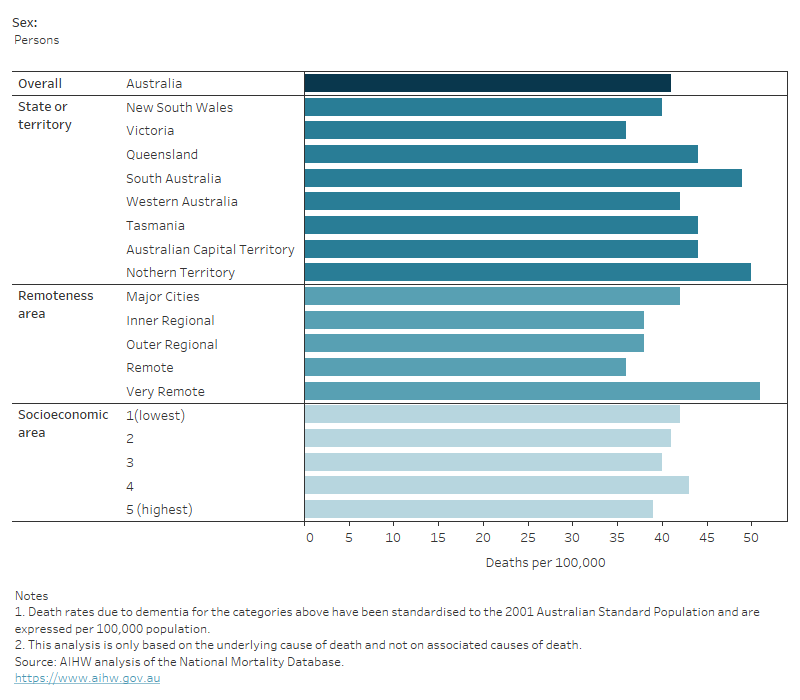
Figure 3.6 shows age-standardised rates of death due to dementia in 2021 by sex, and by different geographic areas and socioeconomic groups. After adjusting for population differences, the age-standardised rate of deaths due to dementia:
- varied across states and territories – ranging from 36 deaths per 100,000 population in Victoria to 50 per 100,000 population in the Northern Territory
- varied by remoteness – the rate was highest in Very remote (51 deaths per 100,000 population) and lowest in Remote areas (36 per 100,000 population)
- was relatively similar across socioeconomic areas – ranging between 39–43 deaths per 100,000 population (Figure 3.6).
Recent evidence points to the high variability of appropriate dementia care across Australia as well as of dementia awareness among healthcare and aged care workers, which could be impacting where people with dementia die, and when and how dementia deaths are coded (Royal Commission 2019). Information on factors such as place of death, if captured comprehensively, may help to shed some further light on end-of-life care in Australia.
Details on the rate of deaths per 100,000 population are included in Table S3.6.
Figure 3.6: Deaths due to dementia in 2021: age-standardised rates, by sex, and by geographic and socioeconomic areas
This figure shows that dementia death rates varied by state or territory, as well as by remoteness areas, but were similar across socioeconomic areas.
Box 3.2: Where do deaths due to dementia occur?
Place of death, the location or setting in which an individual dies, is an important indicator for end-of-life care. Place of death is currently recorded on either a Death Registration Form or the Medical Certificate of Cause of Death, and it is mostly captured as free text that can vary significantly across jurisdictions (ABS 2021).
In 2021, the ABS released the results of a pilot study in which they developed and applied a methodology to assign a place of death to deaths occurring in 2019, based on data sourced from the Deaths Registration Form and the Medical Certificate of Cause of Death. Deaths were assigned to one of five categories:
- Home/residence
- Residential aged care facility
- Hospital/medical service area
- Other
- Unspecified.
Details of the methodology of assignment can be found on the ABS website.
In 2019, the majority of deaths due to dementia (including Alzheimer’s disease) occurred in a residential aged care facility (77%), with 20% occurring in a hospital or medical service area, and 2.5% occurring in a home or residence. Compared with the other selected causes of death examined, dementia had the highest proportion of deaths occurring in aged care facilities and the lowest occurring in hospitals or medical service areas. This is likely reflective of the higher proportion of people with dementia who reside in aged care facilities at end of life due to disease progression and complex care needs.
ABS (Australian Bureau of Statistics) (2015) Causes of death, Australia, 2013, ABS, Australian Government, accessed 11 July 2022.
ABS (2021) Classifying Place of Death in Australian Mortality Statistics, ABS, Australian Government, accessed 11 July 2022.
ABS (2023). Provisional Mortality Statistics. ABS, Australian Government, accessed 12 July 2023.
Brodaty H, Seeher K and Gibson L (2012) 'Dementia time to death: a systematic literature review on survival time and years of life lost in people with dementia', International Psychogeriatrics, 24(7):1034–1045, doi:10.1017/S1041610211002924.
Dementia Australia (2019) The later stages of dementia, Dementia Australia, accessed 1 August 2021.
Gao L, Calloway R, Zhao E, Brayne C, Matthews FE and Medical Research Council Cognitive Function and Ageing Collaboration (2018) 'Accuracy of death certification of dementia in population-based samples of older people: analysis over time', Age and Ageing, 47(4):589–594, doi:10.1093/ageing/afy068.
NHMRC (National Health and Medical Research Council) (2019) Boosting dementia research grants, NHMRC, Australian Government, accessed 1 August 2021.
PHE (Public Health England) (2016) Data analysis report: dying with dementia, PHE, UK Government, accessed 17 August 2022.
Royal Commission (Royal Commission into Aged Care Quality and Safety) (2019) Interim Report: Neglect, Royal Commission, Australian Government, accessed 17 August 2022.


