How do care needs of people with dementia differ by place of residence?
This page describes how the care needs of people with dementia differ between people living in the community and those living in cared accommodation (such as a residential aged care facility), including differences in:
It also includes information on assistance needs and the source of assistance for people with dementia living in the community.
The data presented are from the 2018 Australian Bureau of Statistics’ Survey of Disability, Ageing and Carers (SDAC), which surveys a sample of people with dementia in urban and rural areas of Australia living in the community and living in a number of different types of cared accommodation. On this page, ‘people with dementia’ refers to Australians with dementia in 2018 from the SDAC. Expand the following section, Survey of Disability, Ageing and Carers (SDAC) 2018 and measures of disability, for more information on the SDAC and its limitations for reporting on people with dementia.
Some of the statistics presented in this report are also shown in Aged care and support services used by people with dementia. However, the statistics there are slightly different because they are based on aged care administrative datasets (rather than the SDAC 2018) and are presented for people with dementia who were assessed for using government-subsidised aged care services, and those who are living in permanent residential aged care.
If you are interested in the care needs of people with dementia using aged care services refer to Aged care and support services used by people with dementia.
For demographic information and/or additional information on the assessed needs of people with dementia in Australia refer to Prevalence of dementia and Dementia in priority groups (including First Nations people, people from culturally and linguistically diverse (CALD) backgrounds, people with intellectual disabilities, veterans and the LGBTIQ+ community).
The 2018 SDAC provides detailed information on Australians who belong to one or more of the following groups:
- people with disability
- older people (those aged 65 years and over)
- unpaid carers of people with disability, or a long terms health condition or older people.
The SDAC surveyed people in urban and rural areas of Australia, in 2 distinct groups, referred to in this report as those living in:
- the community: includes people living in private dwellings and self-care retirement villages. This is referred to as ‘households’ in the SDAC.
- cared accommodation: includes people living in a cared accommodation facility for a minimum of 3 months where there is 24-hour access to assistance for personal and/or medical needs, and all meals are provided. This includes hospitals, residential aged care facilities, hostels, cared components of retirement villages and other ‘homes’, such as group homes for people with disability. The vast majority (98%) of people with dementia in cared accommodation in the SDAC were living in residential aged care facilities (government-subsidised and non-government-subsidised facilities) (Table S5.9).
As the SDAC relies on self-reported information about a respondents’ health status for those living in the community, the number of people with dementia as reported by the SDAC is likely to be an underestimate. The information on dementia collected by the SDAC requires people to be formally diagnosed, and this diagnosis being reported by the respondent. This may be a particular issue for people with dementia who are living in the community as they either have not yet been formally diagnosed with dementia, are not aware they have it or are unwilling to disclose it. Further, for those who do not have a carer, they may be unable to respond to the survey. The probable underestimate of people with dementia based on the findings of the SDAC should be considered when interpreting the information on people with dementia in this webpage.
In this webpage, there are a number of SDAC estimates where the relative standard errors are between 25% and 50%. These estimates are noted in the figures and should be used with caution.
Disability levels in the SDAC
In the SDAC, respondents with disability include those who have impairments or limitations which restrict their ability to undertake everyday activities, and has lasted, or is expected to last, for at least 6 months. To measure the extent of disability, the SDAC classified limitations into 4 groups based on a persons’ experience in undertaking core activities (self-care, communication and mobility):
mild: the person needs no help and has no difficulty with any of the core activity tasks, but uses aids or equipment for core tasks, or has other limitations with core tasks (such as difficulty walking short distances, unable to easily bend over or needs help with using public transport).
moderate: the person needs no help, but has difficulty with a core activity task.
severe: the person sometimes needs help with a core activity task, and/or has difficulty understanding or being understood by family or friends, or can communicate more easily using non-spoken forms of communication.
profound: the person is unable to do, or always needs help with, a core activity task.
A person's overall level of core activity limitation is determined by their highest level of limitation in these activities.
In the SDAC it is not possible to determine if dementia was the only cause of disability. There may be other co-existing conditions contributing to the disability level of a person with dementia. Further, a person with dementia may be considered to have no disability if they are still able to undertake everyday activities.
The SDAC also classified people as having a ‘schooling/employment restriction only' if someone reported no limitations with any of the core activities but reported having difficulty with schooling and/or employment activities. For the purposes of this report, this restriction was not included as a disability level.
More information on the SDAC is found in the Technical notes.
Level of disability
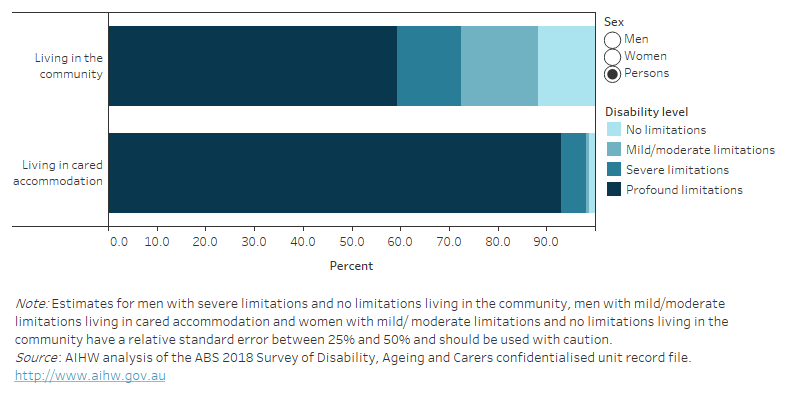
According to the SDAC, in 2018, 59% of people with dementia living in the community and 93% of people with dementia living in cared accommodation were considered to have profound limitations. This means they are unable to do, or always need help with self-care, communication and/or mobility (Figure 5.1). This demonstrates the significant impact dementia has on physical and cognitive functioning, and the need for continued care and support that living in cared accommodation provides.
Among people with dementia living in the community, 58% of men and 61% of women had profound limitations, and 14% of men and 12% of women had severe limitations. A greater percentage of men with dementia living in the community had mild/moderate limitations (18%) compared with women living in the community (13%).
In comparison, the majority of men and women living in cared accommodation had profound limitations (92% and 93%, respectively).
Figure 5.1: Level of disability among people with dementia in 2018: percentage by sex and place of residence
Figure 5.1 is a stacked bar graph showing the percentage of people with dementia by disability level in 2018 (no limitations, mild/moderate limitations, severe limitations and profound limitations) for men, women and persons by place of residence (living in the community or in cared accommodation). Around 92% of men and 93% of women with dementia living in cared accommodation have profound limitations, whereas 58% of men and 61% of women with dementia living in the community have profound limitations. Around 12% of people with dementia living in the community had no limitations and 16% had mild/moderate limitations.
Co-existing health conditions
People with dementia often have a number of co-existing health conditions, which can increase or complicate their care needs. Based on the SDAC for the year 2018, we report on co-existing conditions, comparing people living in the community with those living in cared accommodation.
Of those with dementia who reported having multiple health conditions, dementia was reported as the main condition for a greater proportion of people living in cared accommodation (66%) than people living in the community (52%) (Table S5.2).
On average, people with dementia living in the community have 5 long-term health conditions
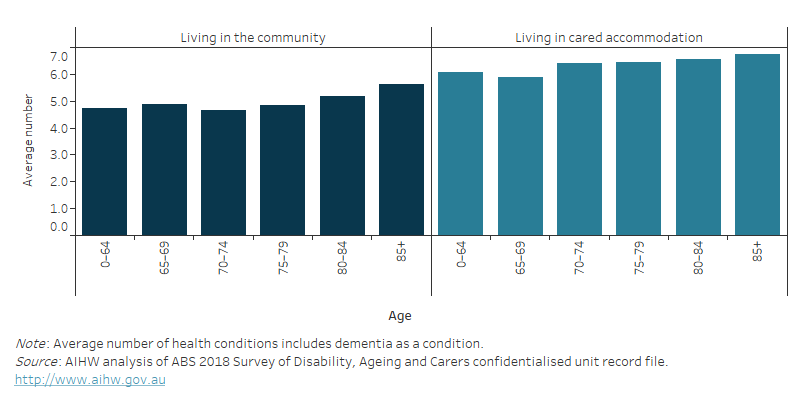
According to the SDAC, people with dementia living in the community had an average of 5.1 long-term health conditions (including dementia) (Figure 5.2). This was lower than for those living in cared accommodation (6.6 conditions). Long-term health conditions are defined as diseases or disorders lasting (or likely to last) for 6 months or more, and conditions that are periodic or episodic in nature (for example, asthma or epilepsy) where the attack or relapse has occurred in the last 12 months (ABS 2019).
There was little difference between men and women with dementia but the average number of conditions generally increased with age, regardless of where they lived. People with younger onset dementia (aged under 65) living in the community had, on average, 4.7 health conditions and those living in cared accommodation had 6.1 health conditions. Among people aged 85 and over with dementia, this increased to 5.6 conditions for those living in the community and 6.8 conditions for those in cared accommodation.
Figure 5.2: Average number of health conditions among people with dementia in 2018: by age and place of residence
Figure 5.2 is a bar graph showing the average number of long term health conditions among people with dementia in 2018 by place of residence and age. The average number of health conditions increased with age both among those living in the community and those living in cared accommodation. In each age group, people with dementia living in cared accommodation had more health conditions on average that those with dementia living in the community.
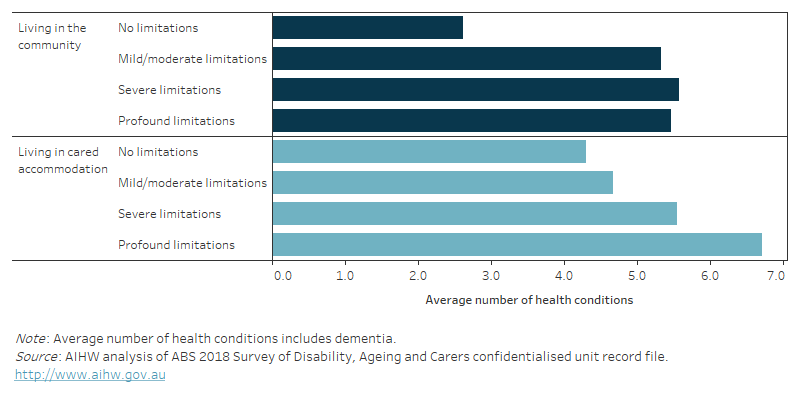
Among people with dementia living in the community, there was little variation in the average number of health conditions across disability levels (with the exception of people with no limitations) (Figure 5.3). Whereas, the average number of health conditions increased with increasing level of disability among people living in cared accommodation.
The average number of health conditions was higher for people with profound limitations living in cared accommodation (average of 6.7) than among people with profound limitations living in the community (average of 5.5 conditions). The majority of people with profound limitations were living in cared accommodation, reflecting their need for extensive care.
The average number of health conditions was fairly similar between people with mild/ moderate or severe limitations living in the community to those in cared accommodation.
Figure 5.3: Average number of health conditions among people with dementia in 2018: by level of disability and place of residence
Figure 5.3 is a bar graph showing the average number of long term health conditions among people with dementia in 2018 by place of residence and disability level. The average number of health conditions increased with increasing level of disability among people living in cared accommodation. For those with dementia living in the community, there was little variation in the average number of health conditions across disability levels (except for people with no limitations, where the average number of health conditions was much lower).
Common co-existing health conditions
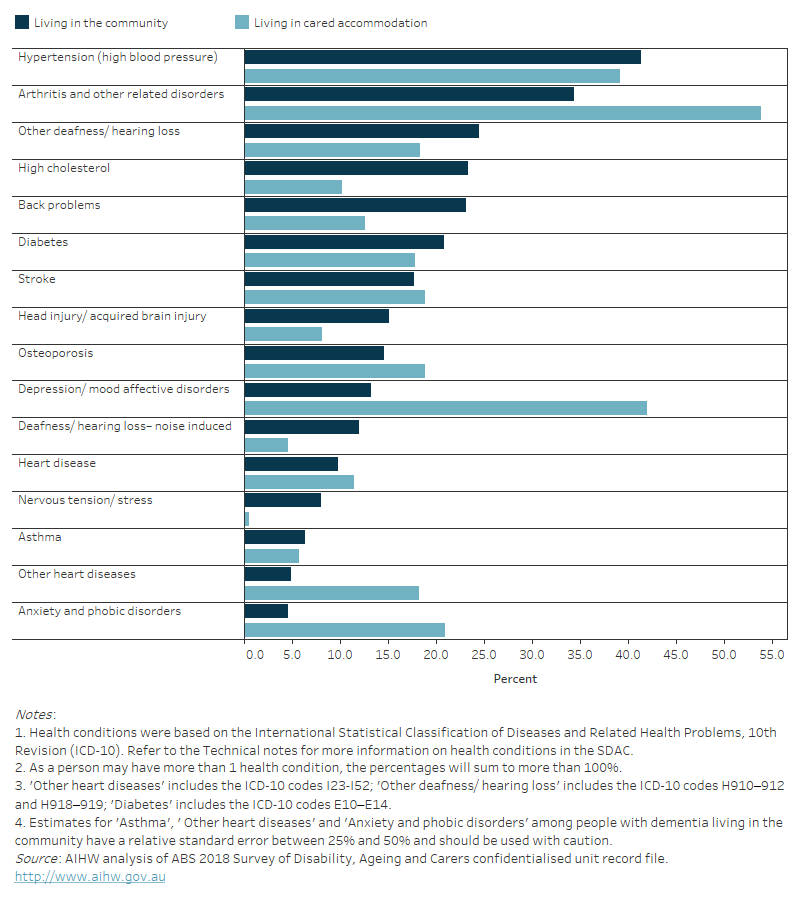
According to the SDAC, the most common co-existing health conditions in people with dementia in 2018 varied by whether they were living in the community or in cared accommodation (Figure 5.4).
Of those with dementia living in the community:
- 41% also had hypertension (high blood pressure) – this was similar to people living in cared accommodation (39%)
- 34% also had arthritis and related disorders – this was lower than those living in cared accommodation (54%)
- 25% also had other hearing loss or deafness (that was not noise induced) – this was higher than those living in cared accommodation (18%)
- 23% also had high cholesterol – this was higher than those living in cared accommodation (10%)
- 23% also had back problems – this was higher than those living in cared accommodation (13%).
Depression and anxiety & phobic disorders were substantially higher among people with dementia living in cared accommodation (42% and 21%, respectively) than in the community (13% and 4.6%, respectively).
Head injury/acquired brain injury, noise induced hearing loss and nervous tension/stress were more common among people with dementia living in the community (15%, 12% and 8.1%, respectively) than in cared accommodation (8.2%, 4.6% and 0.5%, respectively).
Figure 5.4: Common health conditions among people with dementia in 2018: percentage by place of residence
Figure 5.4 is a bar graph showing the percentage of people with dementia in 2018 who had other health conditions by place of residence and health condition. Hypertension and Arthritis & other related disorders were the most common coexisting health conditions among people with dementia living in the community as well as those living in cared accommodation. Head injury/acquired brain injury, High cholesterol, Back problems, Noise-induced hearing loss, and Nervous tension/stress were more common among people with dementia living in the community than those in cared accommodation. Depression/mood affective disorders and Anxiety & phobic disorders were substantially higher among people with dementia living in cared accommodation than in the community.
Box 5.1: Information on co-existing health conditions among people with dementia from other data sources
Data on the co-existing health conditions of people with dementia are available from a number of data sources. They include the SDAC, as well as administrative data from aged care services (presented in Aged care and support services used by people with dementia).
Information on co-existing health conditions for all people with dementia who were assessed for the use of government-subsidised aged care services is available from the National Screening and Assessment Form (NSAF) as well as from the Aged Care Funding Instrument (ACFI) for people with dementia living in permanent residential aged care. The profile of co-existing health conditions from these sources was similar to the profile seen using the SDAC for some conditions. However, there are a number of differences that are likely due to variations in how health condition information is collected between these sources, as well as differences in the group of people with dementia examined.
If you are interested in co-existing health conditions among people with dementia using aged care services refer to Aged care assessments and Residential aged care. For more detail on how health condition information is collected from each of these data sources refer to Technical notes.
Assistance needs for people with dementia living in the community
People with dementia often require care in various activities of daily living. This section presents the broad assistance needs of people with dementia living in the community, how needs vary by place of residence and the source of assistance for people with dementia living in the community as reported in the 2018 SDAC.
Carers of people with dementia provides information on the informal carers, who provide support and assistance for people with dementia living in the community, and Residential aged care provides information on assistance needs of people with dementia living in residential aged care.
Broad assistance needs
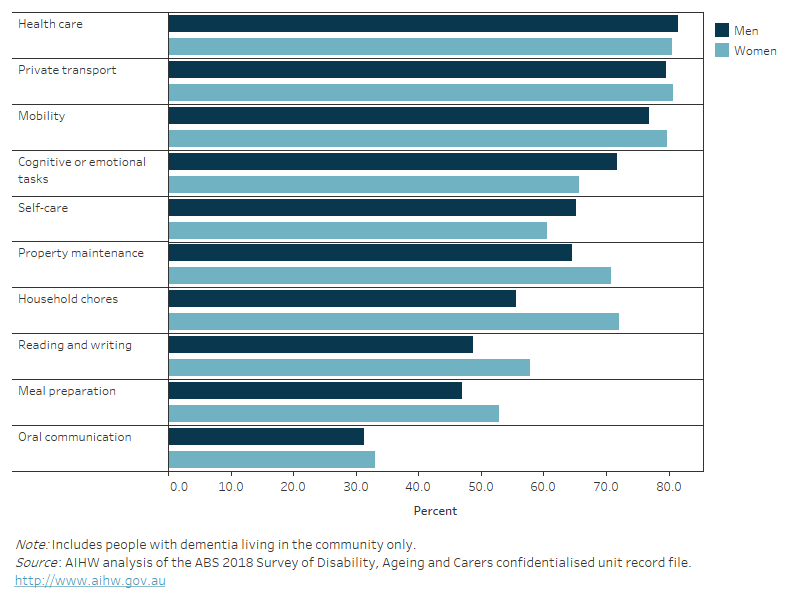
Based on the SDAC, more than three-quarters of people with dementia living in the community who required assistance in 2018 required assistance in 3 activities – health care (81%), private transport (80%) and mobility (78%) (Table S5.6).
When looking at the assistance needs for the 3 core activities individually – self-care, communication and mobility – men and women living in the community were most likely to need assistance with mobility (77% of men and 80% of women) (Figure 5.5).
Women were more likely to need assistance with household chores (56% of men compared with 72% of women). For all other activities, there was little difference in the proportion of men and women living in the community who required assistance.
Figure 5.5: People with dementia living in the community who required assistance in 2018: percentage by sex and activity
Figure 5.5 is a bar graph showing the percentage of people with dementia living in the community who required assistance in 2018 by sex and the type of activity they required assistance with. The majority required assistance with health care, private transport and mobility. Women were more likely to need assistance with household chores, but for all other activities, there was little difference by sex.
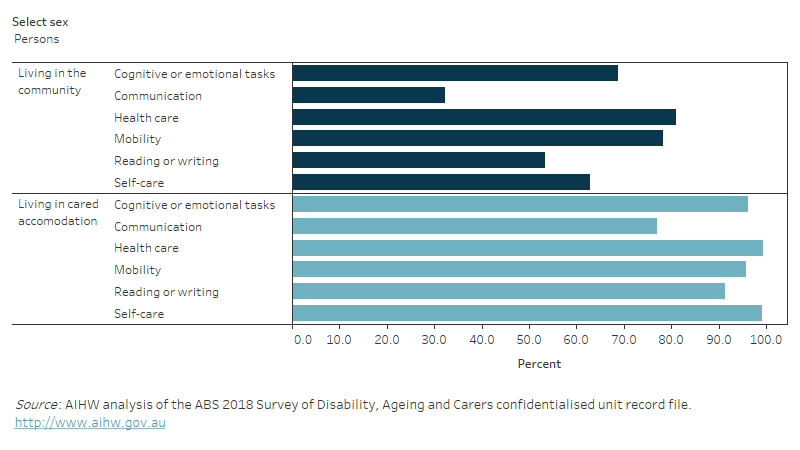
Unsurprisingly, for each activity the proportion of people with dementia who needed assistance was lower for those living in the community than those living in cared accommodation and there was little difference by sex (Figure 5.6). This reflects the greater care needs of people living in cared accommodation, such as permanent residential aged care facilities.
The greatest difference was in the need for assistance with communication; 32% of people with dementia living in the community compared with 77% of those living in cared accommodation. This was followed by assistance with reading or writing (53% in the community and 91% in cared accommodation) and self-care (63% in the community and 99% in cared accommodation).
Note, meal preparation, private transport, property maintenance and household chores are not included as these activities are provided for people living in cared accommodation.
Figure 5.6: People with dementia who required assistance in 2018: percentage by sex, activity and place of residence
Figure 5.6 is a bar graph showing the percentage of people with dementia who required assistance in 2018 by sex, place of residence and the type of activity they required assistance with. The percentage of men and women with dementia who needed assistance in each activity was lower among those living in the community than those living in cared accommodation. There was little difference by sex. The greatest difference was in the percentage who needed assistance with communication, followed by assistance with reading or writing and self-care.
Overall source of assistance
Assistance from informal sources (such as family and friends) as well as from formal sources (such as dementia-specific, disability support and/or aged care services) are essential for people with dementia living in the community.
According to the SDAC, over 1 in 3 people with dementia (36%) who were living in the community in 2018 relied on informal assistance only (Table S5.7).
For information on how the source of assistance varies among people with dementia born in non-English speaking countries refer to Dementia among people from culturally and linguistically diverse backgrounds. For information on informal carers of people with dementia refer to Carers of people with dementia.
Source of assistance in core and other activities
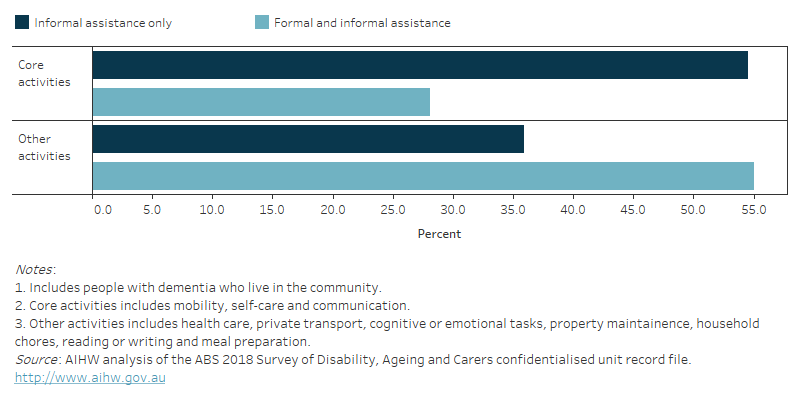
The SDAC grouped activities in which people require assistance into 2 groups:
- Core activities – this includes self-care, communication and mobility. People with more severe limitations (severe or profound limitations) require assistance with one or more of these activities.
- Other activities – this includes private transport, property maintenance, household chores, reading or writing, health care, cognitive or emotional tasks, and meal preparation.
If we look at the source of assistance people with dementia living in the community were receiving by whether this was for core activities or other activities:
- 55% received assistance in core activities from informal sources only – this was higher than the percentage who received informal assistance for other activities (36%).
- 28% received assistance in core activities from a combination of informal and formal sources – this was lower than the percentage who received a combination of informal and formal assistance with other activities (55%) (Figure 5.7).
The high percentage of people with dementia requiring support from informal carers demonstrates the importance and responsibilities that informal carers (such as family and friends) have for caring for an individual with dementia. Refer to Carers of people with dementia for more information on informal carers.
Figure 5.7: People with dementia living in the community who require assistance in 2018: percentage by source of assistance for core and other activities
Figure 5.7 is a bar graph showing the percentage of people with dementia who were living in the community and required assistance in 2018 by source of assistance for core and other activities. Core activities include self-care, communication and mobility. Other activities include private transport, property maintenance, household chores, reading or writing, health care, cognitive or emotional tasks, and meal preparation. Over half of people with dementia who were living in the community and required assistance were receiving support with core activities from informal sources only (such as family and friends). Over one-third were receiving support with other activities from informal sources only.
Australian Bureau of Statistics (ABS) (2019) Disability, Ageing and Carers, Australia: Summary of Findings, 2018– Explanatory notes, ABS, Australian Government, accessed 17 January 2020.


