National dementia behaviour support programs
Behaviours and psychological symptoms of dementia (BPSD) are often associated with complex care needs, with those affected requiring support from a number of health teams and professionals. BPSD is associated with carer stress, increased duration of hospitalisation and greater likelihood of placement in a residential care facility (NSW Health 2013). In Australia, there are a range of services available to support people experiencing BPSD, including programs supported by funding from the Australian Government.
This page provides information and statistics on:
Dementia Support Australia
Dementia Support Australia (DSA) is a service led by HammondCare’s Dementia Centre and funded by the Australian Government. Learn more about DSA’s aims and services in Overview of dementia support services and initiatives.
DSA provides key national support services that can be accessed independently and provide tiered levels of support for people with dementia, their carers and aged care providers. These include:
- Dementia Behaviour Management Advisory Service (DBMAS)
- Severe Behaviour Response Teams (SBRT)
- Needs Based Assessment program, which determines eligibility for the Specialist Dementia Care Program.
Currently DSA are the only national data source that collect Neuropsychiatric Inventory (NPI) information about people who experience BPSD, however this only captures people accessing their services. As such, DSA data are not representative of all people living with dementia or BPSD in Australia.
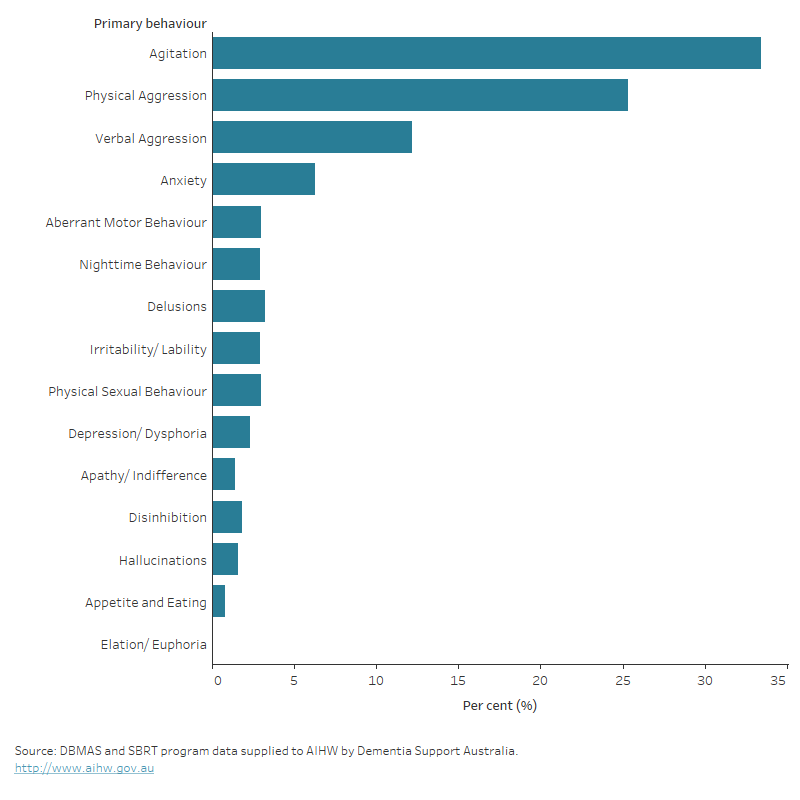
At intake and case closure, DSA routinely administers the Neuropsychiatric Inventory – Questionnaire (NPI-Q) and Neuropsychiatric Inventory – Nursing Home (NPI-NH) for DBMAS and SBRT clients respectively. Both instruments assess BPSD across three shared metrics: the total number of behaviours exhibited by the client, the total severity of these behaviours, and the total distress these behaviours cause formal and informal caregivers. In addition, the primary behaviour (indicating the main reason for referral) of the person with dementia is recorded during the referral process. Among assessments completed between July 2022 and June 2023, agitation was the most commonly recorded primary behaviour, accounting for one third (33%) of referrals. This was followed by physical aggression (25%), verbal aggression (12%) and anxiety (6.3%) (Figure 15.1a).
Figure 15.1a: Dementia Support Australia referrals between July 2022–June 2023, percentage by primary behaviours
Horizontal bar graph showing that agitation was the most recorded primary behaviour among assessments completed between July 2022 and June 2023, followed by physical aggression and verbal aggression.
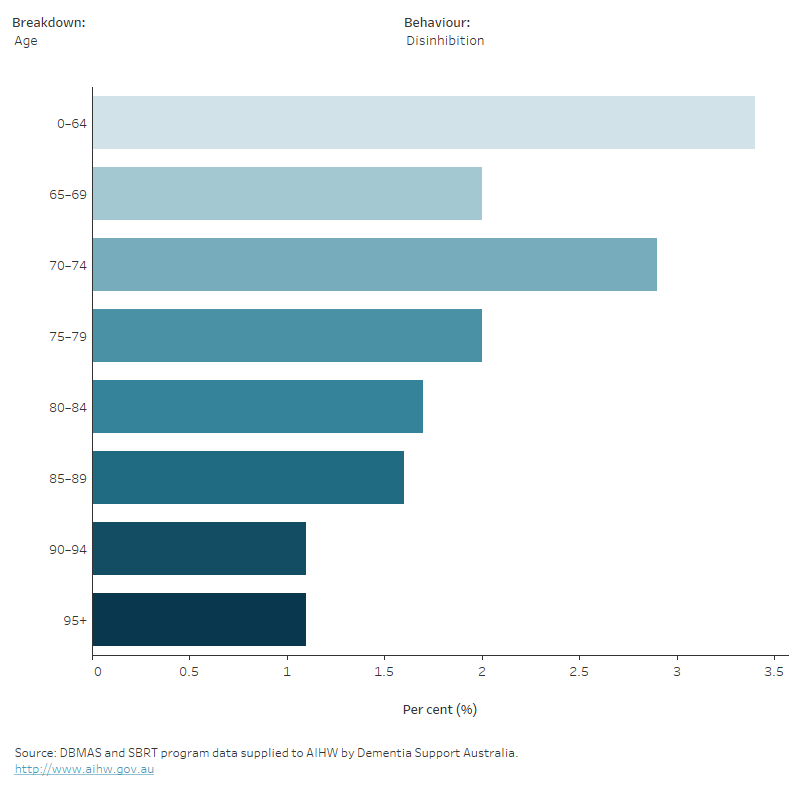
Primary behaviours varied by age and sex
Primary behaviours varied by age and sex. While there were no clear trends by age group, some primary behaviours were more common by sex. Male clients were more likely to be referred for physical aggression, disinhibition or physical sexual behaviour than female clients. While most other primary behaviours, including anxiety, delusions and depression/dysphoria appeared more commonly in referrals of female clients compared to male clients (Figure 15.1b).
Figure 15.1b: Dementia Support Australia referrals between July 2022–June 2023, percentage of primary behaviours by age and sex
Horizontal bar graph displaying percentage of symptoms by symptom type, age, and sex. Most primary behaviours occurred more commonly in referrals of female clients compared to male clients.
Primary behaviours varied between Dementia Support Australia’s behaviour support programs
The DBMAS is a program designed to provide proactive support early on, where there is less risk related to behaviour. For people living with dementia who are experiencing severe behaviour and psychological symptoms, the SBRT is recommended.
Between July 2022 and June 2023, clients assessed for DBMAS and SBRT varied in primary behaviour. The majority of referrals resulting in an SBRT assessment recorded physical aggression (63%) or agitation (20%) as a primary behaviour. While physical aggression and agitation were also the leading recorded primary behaviours at referral of a DBMAS assessment, they accounted for a lower proportion (combined 55%) of primary behaviours recorded at referral, compared to the same behaviours in SBRT.
| Primary behaviour | DBMAS | SBRT |
|---|---|---|
Agitation | 35.3 | 19.9 |
Physical Aggression | 19.8 | 63.0 |
Verbal Aggression | 13.1 | 5.5 |
Anxiety | 7.1 | 1.2 |
Aberrant Motor Behaviour | 3.2 | 1.5 |
Delusions | 3.5 | 1.2 |
Nighttime Behaviour | 3.2 | 1.1 |
Irritability/ Lability | 3.2 | 1.1 |
Physical Sexual Behaviour | 2.9 | 3.8 |
Depression/ Dysphoria | 2.5 | 0.6 |
Disinhibition | 1.9 | 0.8 |
Apathy/ Indifference | 1.5 | 0.2 |
Hallucinations | 1.8 | 0.3 |
Appetite and Eating | 0.9 | 0.0 |
Elation/ Euphoria | 0.0 | n.p. |
Note: n.p. – Not available for publication. Estimate is considered to be unreliable.
Source: DBMAS and SBRT program data supplied to AIHW by Dementia Support Australia.
Severe BPSD requires specialist care
Although rare, BPSD can be severe enough that highly specialised care is needed above that provided by SBRT. For clients requiring specialist accommodation, care and support, the Needs Based Assessment Service (NBA) is recommended to assess eligibility for Specialist Dementia Care Program (SDCP) placement. As the prevalence of people experiencing BPSD decreases as severity of the symptoms increase, there is a much smaller number of NBA referrals when compared with the SBRT and DBMAS programs. Between July 2022 and June 2023, a total of 291 NBA referrals were assessed.
The NBA program assesses eligibility with three key principles:
- Behaviours and psychological symptoms are primarily the result of dementia.
- Symptoms are severe or very severe.
- Symptoms have remained non-responsive to adequate trials of treatment, including non-pharmacological interventions and other specialist programs.
Assessments may be rated ineligible for a number of reasons, including severity not being evaluated as high enough. Conversely, assessments may be rated as ineligible due to behaviours being too severe for Specialist Dementia Care Program (SDCP) placement. Of the referrals between July 2022 and June 2023, 1 in 3 (33%) were rated ineligible. Of these, around a quarter (26%) were rated ineligible due to extreme behaviours.
Overall Neuropsychiatric Inventory (NPI) scores improved following engagement with programs
While the information presented above focuses on the primary behaviour clients present with, clients can experience multiple behaviours at once. Between January 2023 and June 2023 DSA clients presented with behaviour symptoms in an average of 5.1 domains out of the 12 NPI domains upon program intake, and 2.7 upon program exit (an overall reduction of 47%) (Table 15.1). This decrease demonstrates the effectiveness of tailored services for BPSD management, and supports findings from a 2021 evaluation on the clinical impact of these programs on neuropsychiatric outcomes (Macfarlane et al. 2021).
Other measures included in the NPI are total severity of behaviours and total distress/disruptiveness of behaviours to formal and informal carers. The average total severity score decreased between clients who were referred to a program compared to clients who were discharged from a program within the six-month period (10.5 compared with 3.9, respectively) (Table 15.2). Similarly, the average total distress score among carers at intake between January 2023 and June 2023 was 14.4, dropping to 4.7 among carers at exit from the program.
Intake | Discharge | |
|---|---|---|
Number of domains | 5.1 | 2.7 |
Total distress | 14.4 | 4.7 |
Total severity | 10.5 | 3.9 |
Source: DBMAS and SBRT program data supplied to AIHW by Dementia Support Australia.
While DSA aims to provide support for people with dementia and their carers, programs also aim to support residential aged care facilities in their support of people experiencing behavioural symptoms. Between January 2023 and June 2023, DSA had an average of 6.5 client referrals per residential aged care facility in Australia and provided support to 2,260 (85%) residential aged care homes in Australia.
Macfarlane S, Atee M, Morris T, Whiting D, Healy M, Alford M and Cunningham C (2021) ‘Evaluating the Clinical Impact of National Dementia Behaviour Support Programs on Neuropsychiatric Outcomes in Australia’, Frontiers in Psychiatry, doi: doi.org/10.3389/fpsyt.2021.652254.
NSW Health (NSW Ministry of Health) & RANZCP (Royal Australian and New Zealand College of Psychiatrists) (2013) Assessment and Management of People with Behavioural and Psychological Symptoms of Dementia (BPSD), NSW Health, accessed 29 March 2022.


