Total health expenditure including hospital services and out-of-hospital services
Key statistics




This page presents the total health expenditure directly attributable to dementia in 2020–21, as well expenditure on hospital services, including:
Total health expenditure
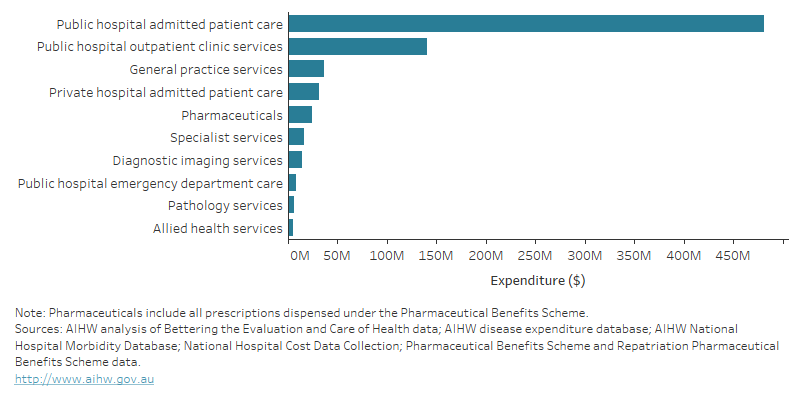
In 2020–21, it was estimated that almost $763 million (or 21% of the total direct health and aged care system expenditure on dementia) was for health expenditure alone. The majority of this expenditure was for:
- hospital-related services – almost $662 million, which included:
- $481 million for public hospital admitted patient care and $31 million for private hospital admitted patient care
- $141 million for outpatient clinics in public hospitals
- $8.6 million for emergency department care in public hospitals.
- GP services – almost $37 million
- pharmaceuticals – just over $24 million (Figure 14.3).
Note that, as with other expenditure estimates in this report, expenditure for public hospital admitted patient care only includes dementia-specific costs of hospital separations (referred to as ‘hospitalisations’) where dementia was a principal or additional diagnosis. It does not include expenditure for the management of conditions other than dementia in estimates for that episode of care, which was 47% of the total cost of hospitalisations with a principal diagnosis of dementia.
Figure 14.3: Estimated health-care system expenditure attributable to dementia in 2020–21: by health-care area
Bar graph showing Australian Government health-care system expenditure attributable to dementia in 2020–21, by health-care area. The graph shows that the majority of expenditure was on public hospital admitted patient care (nearly $481 million) and public hospital outpatient clinic services (nearly $141 million). This was followed by spending on general practice services, private hospital admitted patient care and pharmaceuticals.
Hospital services expenditure
Admitted patient care in public hospitals
In 2020–21, $481 million was spent on public hospital admitted patient care for dementia. Of this, $224 million (or 47%) was for hospitalisations where dementia was the principal diagnosis - or the main reason for admission. The remaining $257 million (or 53%) was for hospitalisations where dementia was an additional diagnosis – where dementia impacted care but was not the main reason for being admitted to hospital. These estimates are for expenditure directly related to dementia and not for the management of other conditions in the same hospitalisation.
How does dementia affect the cost of hospitalisations in public hospitals for common principal diagnoses?
A diagnosis of dementia will influence the cost of a hospitalisation even when it is not the main reason for being admitted to hospital. To understand the costs related to dementia patients in hospital, the average costs of hospitalisations in a public hospital with an additional diagnosis of dementia were compared to those without dementia for 5 common principal diagnoses seen among older people.
The average cost per hospitalisation was greater among people with dementia than people without dementia for each principal diagnosis (Table 14.1).
Principal diagnosis (ICD-10 code) | Average cost, per hospitalisation ($) With dementia | Average cost, per hospitalisation ($) Without dementia | Average cost difference ($) | Rate ratio |
|---|---|---|---|---|
Urinary tract infection, site not specified (N390) | 11,830 | 5,699 | 6,130 | 2.1 |
Pneumonia, organism unspecified (J18) | 14,031 | 9,611 | 4,420 | 1.5 |
Fracture of femur (S72) | 29,879 | 25,023 | 4,856 | 1.2 |
Delirium, not induced by alcohol and other psychoactive substances (F05) | 16,050 | 15,741 | 309 | 1.0 |
Pneumonitis due to solids and liquids (J69) | 13,068 | 12,274 | 793 | 1.1 |
Notes
1. ICD-10–AM refers to the International Classification of Diseases 11th revision Australian Modification.
2. Average cost difference is the average cost per separation with dementia minus the average cost per separation without dementia.
3. Rate ratio is the average cost per separation with dementia divided by the average cost per separation without dementia.
4. Delirium, not induced by alcohol and other psychoactive substances (F05) does not include delirium superimposed on dementia (F051) as this is included in the costs for dementia.
Source: AIHW analysis of National Hospital Morbidity Database and National Hospital Cost Data Collection.
Public hospital outpatient clinics and emergency department care expenditure
In 2020–21, $141 million was spent on non-admitted patient care for dementia in public hospital outpatient clinics, equivalent to 3.8% of the direct health and aged care expenditure attributable to dementia. Services provided in outpatient clinics include; consultations with specialist medical practitioners; allied health and specialist nursing care; diagnostic and other procedures; dispensing of medicines; and some community health services provided by hospitals (AIHW 2023).
A further $8.6 million was spent on emergency department (ED) care in public hospitals, equivalent to 0.2% of the total direct health expenditure on dementia. It is acknowledged that the ED expenditure will be an underestimate, as it relates only to presentations where dementia was recorded as the principal diagnosis. For more information on health condition coding in ED data, refer to the Technical notes.
Expenditure on out-of-hospital services
In 2020–21, over $101 million was estimated to have been spent on out-of-hospital services for dementia, such as GP and specialist services, allied health services, pharmaceuticals, and tests involved in the diagnosis and management of dementia. The expenditure on out-of-hospital services is equivalent to 13% of the total direct health expenditure on dementia and 2.7% of the total health and aged care expenditure on dementia. These estimates are for services where dementia was directly managed and do not include services for patients with dementia where management and treatment related only to their other co-existing health conditions.
Services contributing to the out-of-hospital medical expenditure for dementia were:
- general practice services – almost $37 million
- pharmaceuticals dispensed under the Pharmaceutical Benefits Scheme (PBS) – $24 million
- this includes dementia specific medicines and a range of other medications prescribed for the management of dementia symptoms
- diagnostic imaging – $14 million
- specialist services – over $16 million.
The estimates of expenditure on out-of-hospital medical services include Australian Government costs (under the Medicare Benefits Schedule (MBS) and the PBS), as well as out-of-pocket costs by individuals. The majority of out-of-hospital medical expenditure for dementia (89%, or just under $90 million) was from Australian Government benefits.
Expenditure on medications for dementia
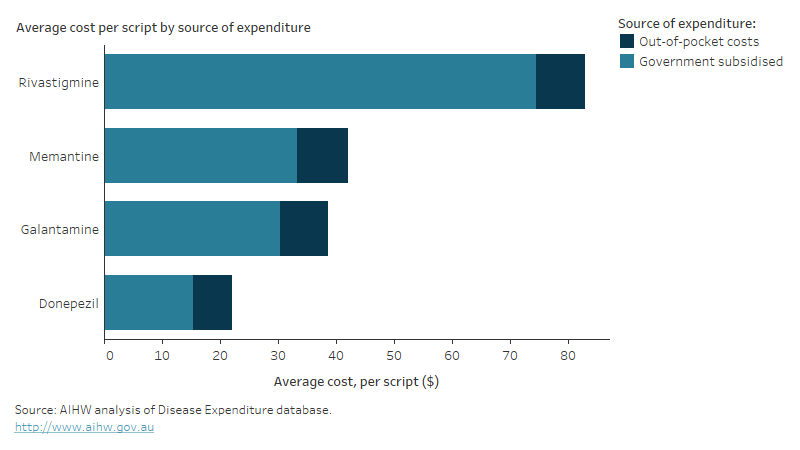
There are 4 dementia-specific medications – Donepezil, Galantamine, Rivastigmine and Memantine – currently subsidised by the Australian Government through the Pharmaceutical Benefits Scheme (PBS) and the Repatriation Pharmaceutical Benefits Scheme (RPBS) for treatment of Alzheimer’s disease. For information on the dispensing of scripts for these medications in Australia in recent years, see Prescriptions for dementia-specific medications.
In 2020–21, the total expenditure on dementia-specific medications was just over $21 million. This included Australian Government expenditure ($17 million, or 78% of expenditure on dementia-specific medications) and out-of-pocket expenses by patients ($4.7 million or 22%). Note, these estimates may include a small amount of expenditure for off-label prescribing of these medications which aren’t captured in the PBS/RPBS.
Of the total expenditure for dementia-specific medications, nearly half was on Donepezil (43% or $9.3 million), followed by Rivastigmine (30% or $6.4 million), Galantamine (13% or $2.8 million) and Memantine (14% or $3.0 million).
The Australian Government subsidised most of the expenditure on each type of dementia-specific medication (Figure 14.4). For patients, the average out-of-pocket cost for a single prescription for a dementia-specific medication was between $7 and $9. The average government subsidised amount per prescription varied substantially - from $15 for Donepezil to $74 for Rivastigmine.
Figure 14.4: Dementia-specific medication expenditure by medication type in 2020–21: average price per script by source of expenditure
Bar graph showing expenditure on four dementia-specific medications (Memantine, Galantamine, Rivastigmine and Donepezil) in 2020–21. The graph shows average cost per script for each medication, by source of expenditure. At $83 per script, Rivastagmine cost approximately twice as much as Memantine and Galantamine and four times as much as Donepezil ($22). The majority of the cost per script was covered by government subsidies for all four medications.
AIHW (Australian Institute of Health and Welfare) (2023) Non-admitted patient activity, AIHW, Australian Government, accessed on 21 February 2024.


