Breastfeeding
On this page:
Introduction
Breastfeeding promotes the healthy growth and development of infants and young children. In Australia, The National Health and Medical Research Council (NHMRC) publishes infant feeding guidelines recommending that infants be exclusively breastfed (Box 1) until around 6 months of age when solid food are introduced. The guidelines also recommend that breastfeeding be continued until 12 months of age and beyond, 'for as long as the mother and child desire' (NHMRC 2015).
There are a range of factors which can influence breastfeeding related to the individual and the environment (Boones et al. 2019; Schmied et al. 2012), and it is important to acknowledge that not every mother chooses to, or is able to, breastfeed.
Box 1: Definition of breastfeeding terms
- Exclusive breastfeeding: The infant receives only breast milk and no other liquids (including water or infant formula), semi-solid and solid foods, except for medications and vitamin and mineral supplements
- Ever breastfed: The infant has been breastfed or received expressed breast milk or colostrum at least once
- Still breastfeeding: The infant receives breast milk and any food or liquid including non-human milk and formula (WHO 2003).
Benefits for mother and child
Breastfeeding provides many benefits for both mother and child. Breastfeeding promotes the healthy growth and development of infants and young children, with benefits extending into adult life (Binns et al. 2016).
Breastfeeding provides infants with a nutrition source that is easy for their digestive systems to absorb, and changes composition over months and years to meet the child’s nutritional, immunological and developmental needs (Kim and Yi 2020). In infants, breastfeeding is also reported as being protective against infections of the ear, respiratory tract and gastrointestinal system, sudden infant death syndrome (SIDS) and malocclusion in baby teeth (Bowatte et al. 2015; Horta and Victora 2013; Hauck et al. 2011; Tham et al. 2015).
In adolescence and adulthood, breastfeeding has been associated with improved cognitive development and a reduction in the risk of living with overweight and obesity and chronic conditions such as diabetes and asthma (Pereyra-Elías et al. 2022; Lefebvre and John 2013; Morris 2018; Miliku and Azad 2018).
Important short- and long-term health benefits have also been seen for mothers (Anatolitou 2012). The immediate maternal benefits of breastfeeding are reduced bleeding and infection after birth, assistance with spacing between pregnancies and maintaining a healthy weight (Victora et al. 2016; Kennedy et al. 1996; Stuebe et al. 2010).
Breastfeeding also provides many long-term benefits such as reduced risk of Type 2 diabetes, cardiovascular disease and breast, ovarian and endometrium cancer (Stuebe et al. 2005; Kirkegaard et al. 2018; Stordal 2023; Stuebe 2009; Babic et al. 2020; Jordan et al. 2017).
Economic benefits
Breastfeeding can have economic benefits at the family level as well as for broader society. For example, families may have no or reduced costs to buy infant formula for the first years after birth (Perez-Escamilla and Segura-Perez 2023). Higher breastfeeding rates lead to lower healthcare costs as breastfeeding protects against a range of diseases.
According to a 2002 study, early weaning was estimated to add around $60 million to $120 million to annual hospitalisation costs for gastrointestinal illnesses, respiratory and ear infection, eczema, and neonatal necrotising enterocolitis in Australian hospitals (Smith et al. 2002).
Environmental benefits
Evidence indicates that feeding with infant formula had almost twice the carbon footprint of breastmilk (Andresen et al. 2022). Infant formulas can negatively impact the environment through production processes related to cattle farming, deforestation, packaging and transportation (Becker and Ryan-Fogarty et al. 2019; Smith 2019). In comparison, breastfeeding uses few resources and produces minimal or no waste.
Barriers and enablers for breastfeeding
There are multiple barriers and enablers that influence breastfeeding practices including biological factors, attitudes, and support.
Demographic factors can influence breastfeeding practices. For example, mothers aged 25 and under were less likely to exclusively breastfeed to 4 months, and more likely to introduce infant formula earlier than mothers aged 35 and older (AIHW 2011).
Additionally, the 2010 Australian National Infant Feeding Survey (ANIFS) showed mothers with lower levels of education, income and socioeconomic status had lower rates of breastfeeding initiation and shorter breastfeeding duration (AIHW 2011).
Mothers with tertiary education qualifications and higher socioeconomic status were more receptive to beneficial health behaviours – such as breastfeeding – and were more likely to seek out support networks (Neves et al. 2021; Boone et al. 2019). These mothers may be more likely to have a supportive workplace and/or home environments for breastfeeding and access to external support systems for breastfeeding issues.
Culturally and linguistically diverse mothers had higher rates of exclusive breastfeeding cessation within 6 months according to the 2010 ANIFS. In a 2012 study of migrant women, participants reported that they struggled to continue breastfeeding while adjusting to life with a baby in a new country (Schmied et al. 2012). Furthermore, migrant women who valued traditional postpartum practices but lacked access to them were more likely to stop breastfeeding (Schmied et al. 2012). Migrant women also had difficulty in accessing culturally appropriate information and support services (Dennis et al. 2018)
Breastfeeding rates are lower among mothers who were living with obesity (body mass index (BMI) of 30 or higher) compared to those within the healthy range (BMI between 18.5 and 24.9) (Hashemi-Nazari et al. 2020). This may be due to a multitude of reasons such as delayed ability to secrete breast milk (Hashemi-Nazari et al. 2020).
Mothers may also cease breastfeeding due to low breast milk supply related to postpartum haemorrhage, mastitis and taking oral contraceptive pills containing oestrogen (Thompson et al. 2010; Pevzner and Dahan 2020). In rare cases, this may be due to the breasts not having enough glandular tissue, which is responsible for producing breast milk (Spatz and Miller 2021).
Research has found that having a baby that was born pre-term or small for gestational age was also associated with lower breastfeeding rates (Lutsiv et al. 2013; Nejsum et al. 2023). These babies potentially have reduced energy and may breastfeed less vigorously and effectively, leading to subsequent weight loss, which negatively impacts the mother’s confidence with breastfeeding (Dooks et al. 2020). Additionally, these babies are taken to neonatal intensive care units (NICU) for observation and treatment which may adversely impact the establishment of breastfeeding due to the introduction of formula at an earlier age (Nejsum et al. 2023). This could lead to higher rates of breastfeeding cessation or formula use.
Women who received any form of support were less likely to stop exclusive breastfeeding before five months than women who did not (Babakazo et al. 2015). Support can take various forms including home visits from trained breastfeeding support providers, helplines, online peer support groups as well as encouragement from partners, family and friends (Babakazo et al. 2015). Having a supportive partner, family and friends can have a positive influence on initiating and sustaining breastfeeding (Snyder et al. 2021).
Access to supportive environments for breastfeeding, particularly workplaces, are an important indicator of continued exclusive breastfeeding (Bradford et al. 2017). Women who had access to working from home, flexible working hours, private space for expressing milk, and paid maternal and paternal leave were more likely to breastfeed for a longer duration (Vilar-Compte et al. 2021).
Breastfeeding strategies and resources
The Australian National Breastfeeding Strategy: 2019 and beyond (the Strategy) recognises breastfeeding is not only an individual woman's issue and aims to provide a framework for integrated, coordinated action to guide Commonwealth, state, territory and local government programs and policies to support mothers, partners, and their infants throughout their breastfeeding journey (CHC 2019).
The key goal of this strategy is to meet the WHO global nutrition target by raising the rate of exclusive breastfeeding in the first 6 months up to at least 50% by 2025.
The Strategy outlines three priority areas to better enable and support breastfeeding. These are:
- Structural enablers
- Settings than enable breastfeeding (for example, breastfeeding-friendly environments which support breastfeeding in the workplace)
- Individual enablers (for example, universal access to breastfeeding support services, particularly for priority groups).
Each of the priority areas are supported by action such as:
- community education and awareness – ensuring clinical care services, support and education are readily available
- increasing the number of settings that are conducive to breastfeeding, such as programs and initiatives that support breastfeeding in the workplace
- a review of regulatory arrangements for restricting the marketing of infant formula products
- increasing health professionals’ education and training surrounding breastfeeding.
- universal access to breastfeeding support services, such as antenatal education about the importance of breastfeeding, and enhanced post-natal support for breastfeeding.
Box 2: Breastfeeding resources and support
The following resources and support services provide breastfeeding and general support and education for parents:
Breastfeeding in Australia
This report will discuss the prevalence of breastfeeding in Australia, focusing on breastfeeding duration and breastfeeding by state or territory, remoteness area and among First Nations mothers.
Box 3: Data sources and methods
This article is primarily based on data from the 2020–21 National Health Survey (NHS) conducted by the Australian Bureau of Statistics (ABS). Between August 2020 and June 2021, the survey was carried out in all Australian states and territories, including urban, rural and remote areas (for more information see National Health Survey 2020–21).
Aboriginal and Torres Strait Islander data reported in this article is from the 2018–2019 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS) which was conducted between July 2018 and April 2019. The survey collected information from First Nations people of all ages in non-remote and remote areas of Australia, including discrete Indigenous communities (for more information see National Aboriginal and Torres Strait Islander Health Survey 2018-2019).
The NHS 2020–21 was collected online during the COVID-19 pandemic and is a break in time series. Data reported can’t be compared to previous years.
The data in this report focuses on infants that were aged 0–3 years at the time of the surveys.
The NHMRC recommends that infants be exclusively breastfed until 6 months of age and then continued breastfeeding alongside suitable complementary foods until 12 months of age and beyond (NHMRC 2015).
According to the 2020–21 National Health Survey (NHS) 96% of infants aged between 0–3 years were breastfed at least once (ever breastfed).
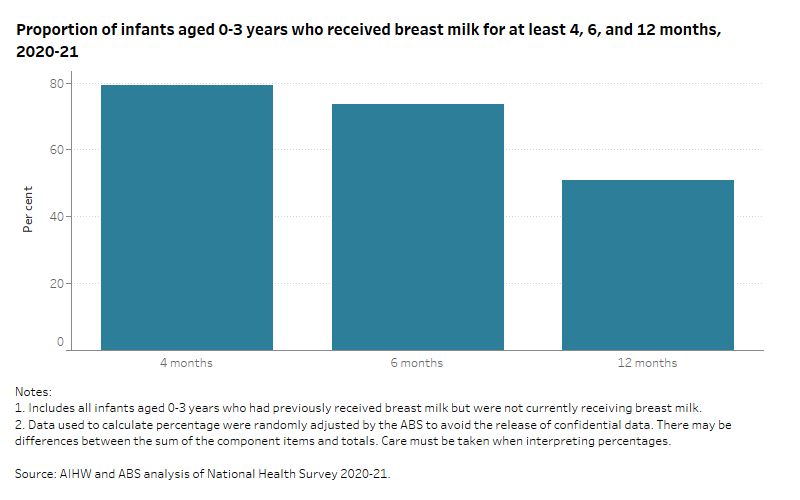
The survey showed that breastfeeding declined as the infants ages increased with:
- 80% of infants received breast milk at 4 months
- 74% received breast milk at 6 months
- 51% received breast milk at 12 months.
The data visualisation (Figure 1) presents data on the proportion of infants aged 0–3 years whoever received breast milk for 4, 6, and 12 months of age, in 2020–21.
Figure 1: Proportion of infants aged 0–3 years who ever received breast milk at 4,6, and 12 months of age, in 2020–21
The bar chart shows the proportion of infants aged 0-3 years that received breast milk decreased as their ages increased.
Exclusive breastfeeding
In 2020–21 the NHS reported that two-thirds (66%) of infants aged 0–3 years were exclusively breastfed at 4 months, and around one-third (35%) at 6 months.
The NHS reported:
- Rates of exclusive breastfeeding ranged across states and territories from 47% in the Australian Capital Territory to 30% in Tasmania
- Exclusive breastfeeding rates also varied across remoteness areas from 38% in Major cities to 27% in Remote areas.
The following data visualisation (Figure 2) presents data on the proportion of infants aged 0-3 years by exclusive breastfeeding status for at least 6 months, and state or territory or remoteness area of participant’s residence, in 2020–21.
Figure 2: Proportion of infants aged 0-3 years by exclusive breastfeeding status for at least 6 months and remoteness area and state or territory, in 2020–21
The bar chart shows that infants living in Major cities and Western Australia had higher rates of exclusive breastfeeding at 6 months.
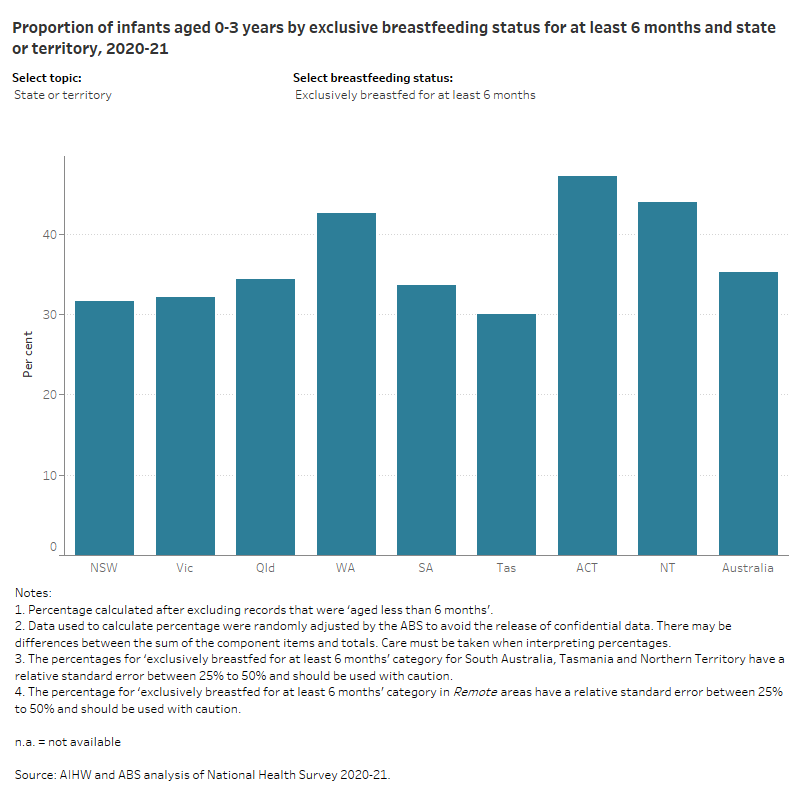
The NHS also reported that in Australia the proportion of infants (0-3 years) who were:
- exclusively breastfed for at least 6 months and continued to breastfeed to 12 months was 2.9%
- exclusively breastfed for at least 6 months but less than 12 months was 33.5%
- not exclusively breastfed for at least 6 months was 63.9%.
These percentages vary from Australia in Figure 2 as data has been randomly adjusted to avoid the release of confidential data.
Introduction to soft, semi-solid or solid foods
The current recommendation is to introduce solids at around 6 months, so that infants can receive nutrients that are essential for growth and development (NHMRC 2015). Introducing solids also helps infants learn how to eat and gives them an experience of new tastes and textures, while developing their teeth and jaw (Borowitz 2021).
The NHS reported that the introduction to soft, semi-solid or solid food varied depending on the age of the infant with 3.3% being introduced at less than 4 months. This increased to 41% at 4 months and 54% at 6 months or later.
Reasons for introduction of food and/or drink other than breast milk
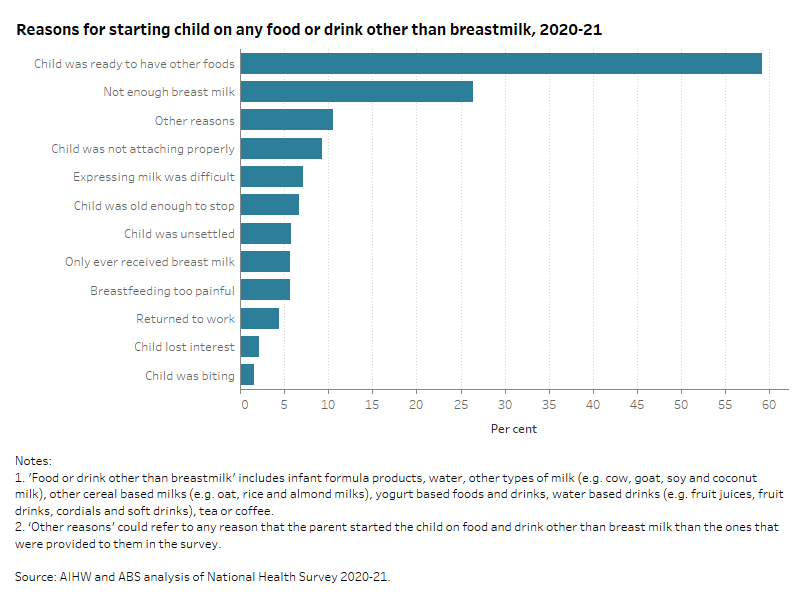
The most common reasons for the introduction of food and/or drink other than breast milk were that:
- the infant was ready to have other foods (59%)
- there was not enough breast milk (26%)
- the infant was not attaching properly (9.3%)
- expressing breast milk was difficult (7.1%).
The following data visualisation (Figure 3) presents the proportion of common reasons for the introduction of food and/or drink other than breast milk, in 2020-21.
Figure 3: Proportion of common reasons for the introduction of food and/or drink other than breast milk, in 2020-21
The bar chart shows that the most common reason for starting food or drink than breast milk was that the child was ready to have other foods
Breastfeeding among First Nations mothers
Breastfeeding practices among First Nations communities have been disrupted by colonisation, prior to which First Nations mothers routinely breastfed their infants, usually for two to four years (Mitchell et al. 2023).
The reduced transmission of cultural breastfeeding practices – and the introduction of non-Indigenous practices such as bottle feeding and the use of infant formula – contribute to the lower breastfeeding rates among First Nations women, especially in urban areas (Springall et al. 2022).
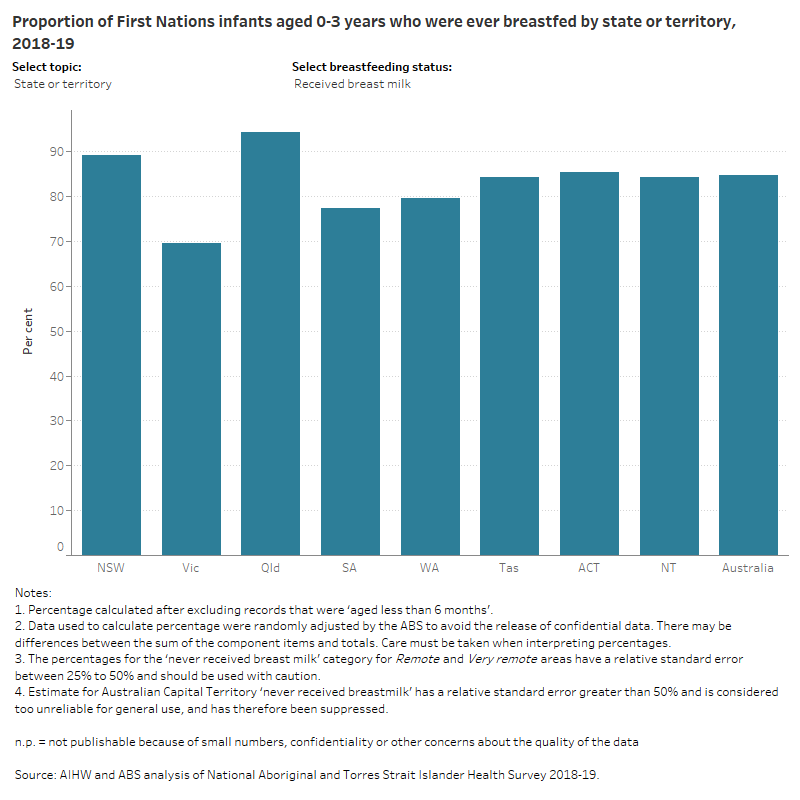
According to the 2018-19 National Aboriginal and Torres Strait Islander Health Survey (NATSIHS), 85% of First Nations infants aged 0-3 years had ever breastfed.
The NATSIHS showed that the rates of breastfeeding varied across state or territories and remoteness areas with:
- The rates of breastfeeding ranged from 94% in Queensland to 70% in Victoria
- Rates of breastfeeding varied across remoteness areas with 94% in Remote areas to 82% in Major cities.
The following data visualisation (Figure 4) presents the proportion of First Nations infants aged 0-3 years who ever breastfed by state or territory and remoteness area, in 2018-19.
Figure 4: Proportion of First Nations infants aged 0-3 years who were ever breastfed by remoteness and state or territory, in 2018-19
The bar chart shows that First Nations infants who lived in Inner regional areas had higher rates of ever receiving breast milk.
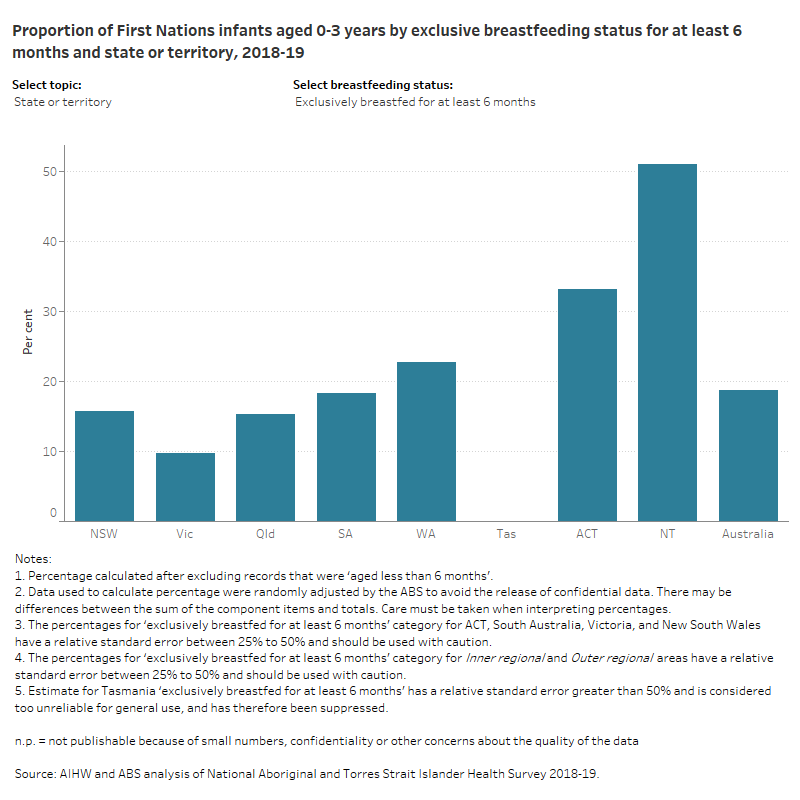
Exclusive breastfeeding among First Nations mothers
The NATSIHS reported that exclusive breastfeeding rates also differed across states or territories and remoteness areas:
- Exclusive breastfeeding rates for 6 months ranged from 23% in Western Australia to 15% in Queensland
- Exclusive breastfeeding rates for 6 months varied from 41% of infants in Very remote to 12% in Major cities.
The following data visualisation (Figure 5) presents data on the proportion of First Nations infants aged 0-3 years by exclusive breastfeeding status for at least 6 months, and state or territory or remoteness area of participant’s residence, in 2018-19.
Figure 5: Proportion of First Nations infants aged 0-3 years by exclusive breastfeeding status for at least 6 months and remoteness area and state or territory, in 2018-19
The bar chart shows that First Nations infants living in Very remote areas had higher rates of exclusive breastfeeding at 6 months.
The NATSIHS also reported that the proportion of First Nations infants (0-3 years) who were:
- exclusively breastfed to 6 months and continued to breastfeed to 12 months was 11.7%
- exclusively breastfed for at least 6 months but less than 12 months was 7.5%
- not exclusively breastfed for at least 6 months was 80.6%.
These percentages vary from Australia in Figure 5 as data has been randomly adjusted to avoid the release of confidential data.
More information
For more information on:
- infant feeding practices for 2010-11 see the Australian National Infant Feeding Survey
- breastfeeding between 2010 and 2014-15 see the Children’s Headline Indicator 4. Breastfeeding
- breastfeeding in 2017-18 see Australia's children, Breastfeeding and nutrition.
ABA (Australian Breastfeeding Association) (2023) Resources, ABA website, accessed 15 March 2023.
AIHW (Australian Institute of Health and Welfare) (2011) 2010 Australian National Infant Feeding Survey: Indicator Results, AIHW, Australian Government, accessed 15 February 2023.
Anatolitou F (2012) ‘Human milk benefits and breastfeeding’, Journal of Pediatric and Neonatal Individualized Medicine, 1(1):11-18, doi:10.7363/010113.
Andresen EC, Hjelkrem AR, Bakken AK, and Andersen LF (2022) ‘Environmental impact of feeding with infant formula in comparison with breastfeeding’, International Journal of Environmental Research and Public Health, 19(11):6397, doi:10.3390/ijerph19116397.
Babakazo P, Donnen P, Akilimali P, Ali NMM and Okitolonda E (2015) ‘Predictors of discontinuing exclusive breastfeeding before six months among mothers in Kinshasa: a prospective study’, International Breastfeeding Journal, 10(19), doi:10.1186/s13006-015-0044-7.
Babic A, Sasamoto N and Rosner BA (2020) ‘Association between breastfeeding and ovarian cancer risk’, JAMA Oncology, 6(6):e200421, doi:10.1001/jamaoncol.2020.0421.
Becker G and Ryan-Fogarty Y (2019) ‘Environmental impact of bottles, teats, and packaging in maternity units’, British Medical Journal, 367:16331, doi:10.1136/bmj.16331.
Binns C, Lee M and Low WY (2016) ‘The long-term public health benefits of breastfeeding’, Asia Pacific Journal of Public Health, 28(1):7-14, doi:10.1177/1010539515624964.
Boone KM, Dynia JM, Logan J and Purtell K (2019) ‘Socioeconomic determinants of breastfeeding initiation and continuation for families living in poverty’, Pediatrics, 144(2):272, doi:10.1542/peds.144.2MA3.272.
Borowitz SM (2021) ‘First bites-why, when, and what solid foods to feed infants’, Frontiers in Pediatrics, 9:654171, doi:10.3389/fped.2021.654171.
Bowatte G, Tham R, Allen KJ, Tan DJ, Lau MXZ, Dai X and Lodge CJ (2015) ‘Breastfeeding and childhood acute otitis media: a systematic review and meta-analysis’, Acta Paediatrica, 104(467):85-95, doi:10.1111/apa.13151.
Bradford VA, Walkinshaw LP, Steinman L, Otten JJ, Fisher K, Ellings A, O'Leary J, and Johnson DB (2017) ‘Creating environments to support breastfeeding: the challenges and facilitators of policy development in hospitals, clinics, early care and education, and worksites’, Maternal and Child Health Journal, 21(12):2188–2198, doi:10.1007/s10995-017-2338-4.
CHC (COAG Health Council) (2019) The Australian National Breastfeeding Strategy: 2019 and Beyond, Department of Health and Aged Care, accessed 15 March 2023.
Dennis CL, Brown HK, Chung-Lee L, Abbass-Dick J, Shorey S, Marini F and Brennenstuhl S (2018) ‘Prevalence and predictors of exclusive breastfeeding among immigrant and Canadian-born Chinese women’, Maternal and Child Nutrition, 15(2):e12687, doi:10.1111/mcn.12687.
DoHAC (Department of Health and Aged Care) (2021) Breastfeeding your baby, Pregnancy, Birth and Baby website, accessed 13 June 2023.
Dooks E, Owens D and Stacey T (2020) ‘The establishment of breastfeeding in the small-for-gestational-age baby’, British Journal of Midwifery, 28(2):2052-4307.
Hashemi-Nazari SS, Hasani J, Izadi N, Najafi F, Rahmani J, Naseri P, Rajabi A and Clark C (2020) ;The effect of pre-pregnancy body mass index on breastfeeding initiation, intention and duration: a systematic review and dose-response meta-analysis’, Heliyon, 6(12):e05622, doi:10.1016/j.heliyon.2020.e05622.
Hauck FR, Thompson JM, Tanabe KO, Moon RY and Vennemann MM (2011) ‘Breastfeeding and reduced risk of sudden infant death syndrome: a meta-analysis’, Pediatrics, 128(1):103-110, doi:10.1542/peds.2010-3000.
Horta BL and Victora CG (2013) ‘Short-term effects of breastfeeding: a systematic review on the benefits of breastfeeding on diarrhoea and pneumonia mortality’, World Health Organisation, Geneva.
Jordan SJ, Na R, Johnatty SE, Wise LA, Adami HO, Brinton LA, Chen C, Cook LS, Dal Maso L, De Vivo I, Freudenheim JL, Friedenreich CM, La Vecchia C, McCann SE, Moysich KB, Lu L, Olson SH, Palmer JR, Petruzella S, Pike MC, Rebbeck TR, Ricceri F, Risch HA, Sacerdote C, Setiawan VW, Sponholtz TR, Shu XO, Spurdle AB, Weiderpass E, Wentzensen N, Yang HP, Yu H and Webb, P. M. (2017) ‘Breastfeeding and endometrial cancer risk: an analysis from the epidemiology of endometrial cancer consortium’, Obstetrics and Gynecology, 129(6):1059–1067, doi:10.1097/AOG.0000000000002057.
Kennedy K, Labbok M and Van Look P (1996) ‘Lactational amenorrhea method for family planning’, International Journal of Gynecology & Obstetrics, 54(1):55–7, doi:10.1016/0020-7292(96)02670-7.
Kim SY and Yi DY (2020) ‘Components of human breast milk from macronutrient to microbiome and microRNA’, Clinical and Experimental Pediatrics, 63(8):301-309, doi:10.3345/cop.2020.00059.
Kirkegaard H, Bliddal M, Støvring H, Rasmussen KM, Gunderson EP, Køber L and Nohr EA (2018) ‘Breastfeeding and later maternal risk of hypertension and cardiovascular disease – the role of overall and abdominal obesity’, Preventive Medicine, 114:140– 148, doi: 10.1016/j.ypmed.2018.06.014.
Lefebvre CM and John RM (2014) ‘The effect of breastfeeding on childhood overweight and obesity: a systematic review of the literature’, Journal of the American Association of Nurse Practitioners, 26(7):386-401, doi:10.1002/2327-6924.12036.
Lutsiv O, Giglia L, Pullenayegum E, Foster G, Vera C, Chapman B, Fusch C and McDonald SD (2013) ‘A population-based cohort study of breastfeeding according to gestational age at term delivery’, The Journal of Pediatrics, 163(5):1283-1288, doi:10.1016/j.jpeds.2013.06.056.
Miliku K and Azad MB (2018) ‘Breastfeeding and the developmental origins of asthma: current evidence, possible mechanisms, and future research priorities’, Nutrients, 10(8):995, doi:10.3390/nu10080995.
Mitchell F, Walker T, Hill K and Browne J (2023) ‘Factors influencing infant feeding for Aboriginal and Torres Strait Islander women and their families: a systematic review of qualitative evidence’, BMC Public Health, 23(297), doi:10.1186/s12889-022-14709-1.
Morris A (2018) ‘Breastfeeding reduces risk of type 2 diabetes mellitus’, Nature Reviews Endocrinology, 14(128), doi:10.1038/nrendo.2018.9.
Nejsum FM, Måstrup R, Torp-Pedersen C, Løkkegaard, ECL, Wiingreen R and Hansen BM (2023) ‘Exclusive breastfeeding: relation to gestational age, birthweight, and early neonatal ward admission. A nationalwide cohort study of children born after 35 weeks of gestation’, PloS One, 18(5):e0285476, doi:10.1371/journal.pone.0285476.
Neves PAR, Barros AJD, Gatica-Domínguez G, Vaz JS, Baker P, and Lutter CK (2021) ‘Maternal education and equity in breastfeeding: trends and patterns in 81 low- and middle-income countries between 2000 and 2019’, International Journal for Equity in Health, 20(1):20, doi:10.1186/s12939-020-01357-3.
NHMRC (National Health and Medical Research Council) (2015) Infant Feeding Guidelines: information for health workers, NHMRC, Australian Government, accessed 15 March 2023.
Noel-Weiss J, Boersma S and Kujawa-Myles S ‘Questioning current definitions for breastfeeding research’, International Breastfeeding Journal, 7(9), doi:10.1186/1746-4358-7-9.
PANDA (Perinatal Anxiety & Depression Australia) (2023) Building your community of care, PANDA website, accessed 13 June 2023.
Pereyra-Elías R, Quigley MA and Carson C (2022) ‘To what extent does confounding explain the association between breastfeeding duration and cognitive development up to age 14? Findings from the UK Millennium Cohort Study’, PloS One, 17(5):e0267326, doi:10.1371/journal.pone.0267326.
Pevzner M, Dahan A (2020) ‘Mastitis while breastfeeding: prevention, the importance of proper treatment, and potential complications’, Journal of Clinical Medicine, 9(8):2328, doi:10.3390/jcm9082328.
Schmied V, Olley H, Burns E, Duff M, Dennis C and Dahlen HG (2012) ‘Contradictions and conflict: a meta-ethnographic study of migrant women’s experiences of breastfeeding in a new country’, BMC Pregnancy and Childbirth, 12(163), doi:10.1186/1471-2393-12-163.
Smith JP (2019) ‘A commentary on the carbon footprint of milk formula: harms to planetary health and policy implications’, International Breastfeeding Journal, 14(49), doi:10.1186/s13006-019-0243-8.
Smith JP, Thompson JF and Ellwood DA (2002) ‘Hospital system costs of artificial infant feeding: estimates for the Australian Capital Territory’, Australian and New Zealand Journal of Public Health, 26(6):543-551, doi:10.1111/j.1467-842x.2002.tb00364.x.
Spatz DL and Miller J (2021) ‘When your breast might not work: anticipatory guidance for health-care professionals’, Journal of Perinatal Education, 30(1):13-18, doi:10.1891/J-PE-D-20-00014.
Springall TL, McLachlan HL, Forster DA, Browne J and Chamberlain C (2022) ‘Breastfeeding rates of Aboriginal and Torres Strait Islander women in Australia: a systematic review and narrative analysis’, Women and Birth, 35(6):624-638, doi:10.1016/j.wombi.2022.02.011.
Stordal B (2023) ‘Breastfeeding reduces the risk of breast cancer: a call for action in high-income countries with low rates of breastfeeding’, Cancer Medicine, 12(4):4616-4625, doi: 10.1002/cam4.5288.
Stuebe AM, Kleinman K, Gillman MW, Rifas-Shiman SL, Gunderson EP & Rich-Edwards J (2010) ‘Duration of lactation and maternal metabolism at 3 years postpartum’, Journal of Women’s Health, 19(5):941–50, doi:10.1089/jwh.2009.1660.
Stuebe AM, Rich-Edwards JW, Willett WC, Manson JE and Michels KB (2005) ‘Duration of lactation and incidence of type 2 diabetes’, Journal of the American Medical Association, 294(20):2601–2610, doi:10.001/jama.294.20.2601.
Synder K, Hulse E, Dingman H, Cantrell A, Hanson C and Dinkel D (2021) ‘Examining supports and barriers to breastfeeding through a socio-ecological lens: a qualitative study’, International Breastfeeding Journal, 16(52), doi:10.1186/s13006-021-00401-4.
Tham R, Bowatte G, Dharmage SC, Tan DJ, Lau MXZ, Dai X, Allen KJ and Lodge CJ (2015) ‘Breastfeeding and the risk of dental caries: a systematic review and meta-analysis’, Acta Paediatrica, 104(467):62-84, doi:10.1111/apa.13118.
Thompson JF, Heal LJ, Roberts CL and Ellwood DA (2010) ‘Women's breastfeeding experiences following a significant primary postpartum haemorrhage: a multicentre cohort study’, International Breastfeeding Journal, 5(5), doi:10.1186/1746-4358-5-5.
Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N and Rollins NC (2016) ‘Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect’, Lancet, 387(10017):475-490, doi: 10.1016/S0140-6736(15)01024-7.
Vilar-Compte M, Hernández-Cordero S, Ancira-Moreno M, Burrola-Méndez S, Ferre-Eguiluz I, Omaña I and Pérez Navarro C (2021) ‘Breastfeeding at the workplace: a systematic review of interventions to improve workplace environments to facilitate breastfeeding among working women’, International Journal for Equity in Health, 20(110), doi:10.1186/s12939-021-01432-3
(World Health Organization) WHO (2003) Global strategy for infant and young child feeding. Geneva: WHO.


