Thermal causes
Citation
AIHW
Australian Institute of Health and Welfare (2023) Thermal causes, AIHW, Australian Government, accessed 27 April 2024.
APA
Australian Institute of Health and Welfare. (2023). Thermal causes. Retrieved from https://www.aihw.gov.au/reports/injury/thermal-causes
MLA
Thermal causes. Australian Institute of Health and Welfare, 06 July 2023, https://www.aihw.gov.au/reports/injury/thermal-causes
Vancouver
Australian Institute of Health and Welfare. Thermal causes [Internet]. Canberra: Australian Institute of Health and Welfare, 2023 [cited 2024 Apr. 27]. Available from: https://www.aihw.gov.au/reports/injury/thermal-causes
Harvard
Australian Institute of Health and Welfare (AIHW) 2023, Thermal causes, viewed 27 April 2024, https://www.aihw.gov.au/reports/injury/thermal-causes
Get citations as an Endnote file: Endnote
This content contains information some readers may find distressing.
If you, or someone you know needs help, contact Lifeline on 13 11 14. Go to the crisis and support services page for a list of support services.
Thermal causes of injury include exposure to smoke, fire and flames as well as contact with hot substances and heat sources, such as hot food and drinks, and household appliances. Burns from bushfires fall in this category.
Children under 5, especially boys, are most at risk of serious thermal injury.
Thermal injuries resulted in:
 5,500 hospitalisations in 2021–22
5,500 hospitalisations in 2021–22
22 per 100,000 population
 120 deaths in 2020–21
120 deaths in 2020–21
0.5 per 100,000 population
This represents 1.0% of injury hospitalisations and 0.9% of injury deaths.
This page summarises data on unintentional thermal injuries only. Intentional injuries and deaths are included under Assault and homicide or Self-harm and suicide.
Thermal causes of injury that led to hospitalisation
In 2021–22:
- 3 in 5 hospitalisations due to thermal causes (60%) were from contact with heat and hot substances
- 2 in 5 hospitalisations due to thermal causes (40%) were from exposure to fire, smoke and flames (Table 1).
Cause | Hospitalisations | % | Rate (per 100,000) |
|---|---|---|---|
Contact with heat and hot substances (X10–19) | 3,352 | 60 | 13.1 |
Contact with hot drinks, food, fats and cooking oils (X10) | 1,010 | 18 | 3.9 |
Contact with hot fluids that are not hot drinks, food, fats and cooking oils (for example, water boiled on stove and hot tap water) (X11–12) | 1,043 | 19 | 4.1 |
Contact with hot household appliances, heating appliances, radiators and pipes (X15-16) | 536 | 9 | 2.1 |
Contact with hot engines, machinery and tools (X17) | 195 | 4 | 0.8 |
Other or unspecified (X13,X14,X18–19) | 568 | 10 | 2.2 |
Exposure to fire, smoke and flames (X00–09) | 2,192 | 40 | 8.5 |
Exposure to a controlled or uncontrolled fire (X00–03) | 901 | 16 | 3.5 |
Exposure to ignition of highly flammable material (X04) | 430 | 8 | 1.7 |
Other or unspecified (X05–09) | 861 | 16 | 3.3 |
Total | 5,544 | 100 | 21.6 |
Notes
- Rates are crude per 100,000 population.
- Percentages and rates may not equal total due to rounding.
- Codes in brackets refer to the ICD-10-AM (11th edition) external cause codes (ACCD 2019).
Source: AIHW National Hospital Morbidity Database.
For more detail, see Data tables B13–14.
Thermal causes of injury that led to death
In 2020–21, two thirds of deaths from thermal causes (66%) were from exposure to fire, smoke and flames (Table 2).
Cause | Deaths | % | Rate (per 100,000) |
|---|---|---|---|
Exposure to a controlled or uncontrolled fire (X00–03) | 64 | 54 | 0.2 |
Other or unspecified exposure to fire, smoke or flames (X04–09) | 15 | 13 | 0.1 |
Contact with heat and hot substances (X10–19) | 11 | 9 | 0.0 |
Elsewhere classified | 29 | 24 | 0.1 |
Total | 119 | 100 | 0.5 |
Notes
- Rates are crude per 100,000 population, calculated using estimated resident population as at 31 December of the relevant year.
- Percentages may not equal 100 due to rounding.
- Codes in brackets refer to the ICD-10 external cause codes (WHO 2011).
Source: AIHW National Mortality Database.
For more detail, see Data tables B19–21.
Trends over time
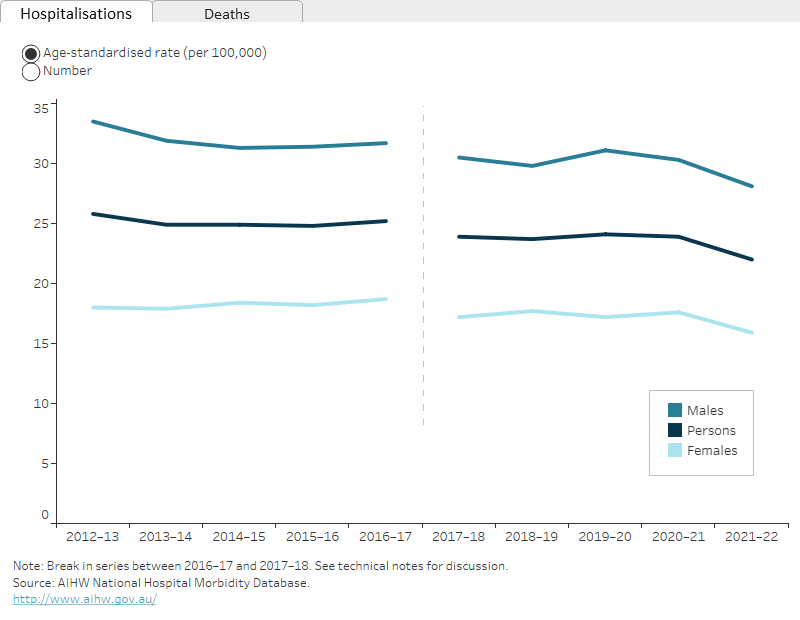
Over the period from 2017–18 to 2021–22, the age-standardised rate of hospitalisations for thermal injuries decreased by an annual average of 2.0%. From 2012–13 to 2016–17 there was an average annual decrease of 0.6%.
There is a break in the time series for hospitalisations between 2016–17 and 2017–18 due to a change in data collection methods (see the technical notes for details).
The rate of deaths from thermal injuries decreased between 2011–12 and 2020–21 by an annual average of 2.4% (Figure 1).
Figure 1: Thermal injury hospitalisations and deaths, by year
2 matching line graphs on separate tabs, 1 tab for hospitalisations and 1 for deaths. The 3 lines represent the trend for males, females, and persons over 10 years. The reader can choose to display rate per 100,000 population or number.
For more detail, see Data tables C1–3 and F1–4.
Seasonal differences
Hospitalisations due to injuries from thermal causes are higher over the colder months (Figure 2).
The interactive display illustrates other seasonal differences in injury hospitalisations.
Figure 2: Seasonal differences in hospitalisations for thermal injuries, 2019–20 to 2021–22
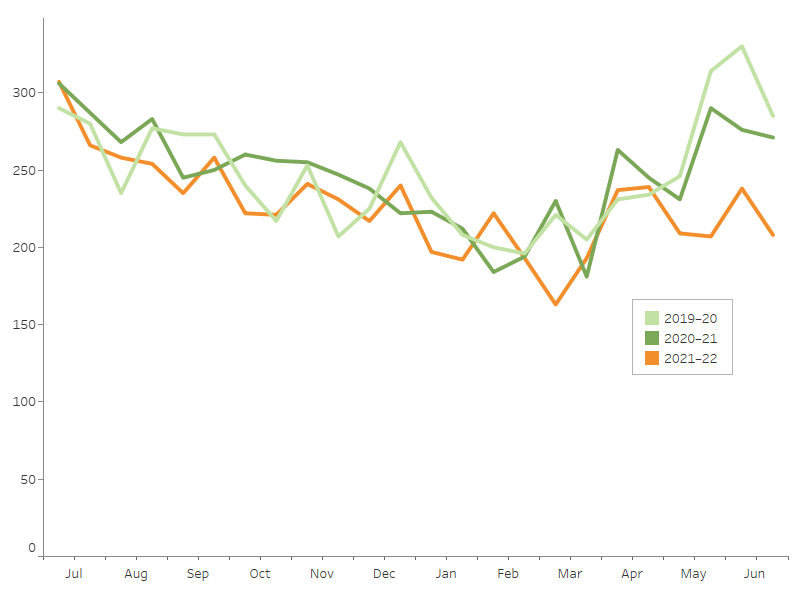
Notes
1. Admission counts have been standardised into two 15-day periods per month.
2. A scale up factor has been applied to June admissions to account for cases not yet separated.
Source: AIHW National Hospital Morbidity Database.
Differences by age and sex
Rates of hospitalisation and death from thermal injuries differ between males and females, especially for certain age groups.
Among thermal injury cases:
- 64% of hospitalisations in 2021–22 were for males
- the age-standardised rates of hospitalisation were 28 per 100,000 males and 16 per 100,000 females
- children aged under 5 had the highest rate of hospitalisation per 100,000 population (Figure 3)
- 67% of deaths in 2020–21 were for males
- the age-standardised rates of death were 0.6 per 100,000 males and 0.3 per 100,000 females.
Figure 3: Thermal injury hospitalisations and deaths, by age group and sex
Column graph representing sex within 6 life-stage age groups. The reader can choose to display either rate per 100,000 population or number, for either hospitalisations or deaths. The default displays rate of hospitalisations for males and females and the reader can also choose to display persons.
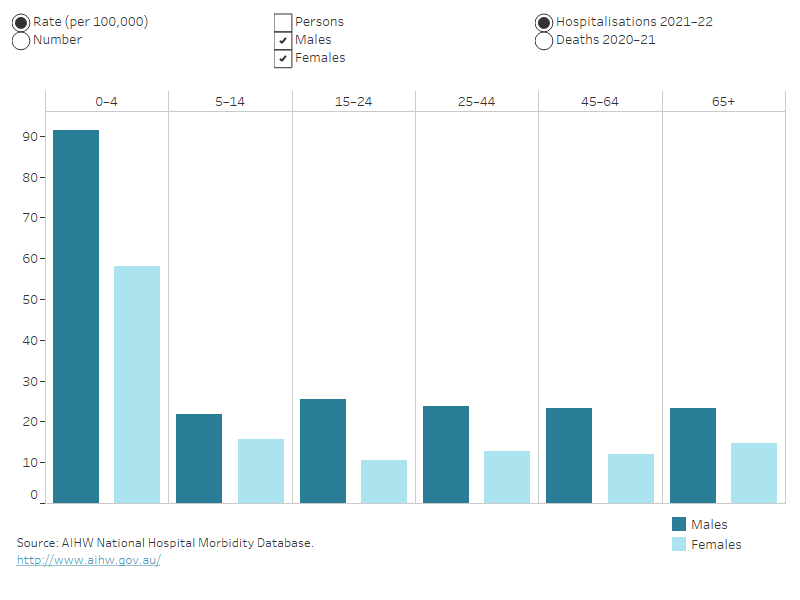
For more detail, see Data tables A1–3 and D1–3.
Severity
There are many ways that the severity, or seriousness, of an injury can be measured. Some of the ways to measure the severity of hospitalised injuries are:
- number of days in hospital
- time in an intensive care unit (ICU)
- time on a ventilator
- in-hospital deaths.
The average number of days in hospital for thermal injuries was higher than the average for all injuries, and the percentages of thermal cases that included time in an ICU and/or involved continuous ventilatory support were higher than for all injuries. The rate of in-hospital death was lower than the average.
|
Thermal causes |
All injuries |
|
|---|---|---|
|
Average number of days in hospital |
5.2 |
4.7 |
|
% of cases with time in an ICU |
3.2 |
2.0 |
|
% of cases involving continous ventilatory support |
2.1 |
1.1 |
|
In-hospital deaths (per 1,000 cases) |
4.7 |
5.9 |
Note: Average number of days in hospital (length of stay) includes hospitalisations that are transfers from 1 hospital to another or transfers from 1 admitted care type to another within the same hospital, except where care involves rehabilitation procedures.
Source: AIHW National Hospital Morbidity Database.
For more detail, see Data tables A12–13.
Body part injured
In 2021–22, the hip and leg was the body part most often identified as the main site of injury in hospitalisations for thermal injuries (Figure 4).
Figure 4: Hospitalisations for thermal injuries, by main body part injured, 2021–22
Outline of a person with labels for body parts related to hospitalisations.
Notes: Body part relates to the main (principal) reason for hospitalisation. Number and percentage of injuries classified as Other, multiple and incompletely specified body regions or Injuries not described in terms of body region not shown—see Data table A11.
Source: AIHW National Hospital Morbidity Database.
Aboriginal and Torres Strait Islander people
In 2021–22, among Aboriginal and Torres Strait Islander people:
- there were 600 hospitalisations for thermal injury (Table 4)
- males were 1.7 times as likely as females to be hospitalised due to thermal causes (age-standardised)
- thermal injury hospitalisation rates were highest in the 0–4 age group (Figure 5).
There were 5 deaths of Indigenous Australians from thermal injuries in 2021–22.
|
|
Males |
Females |
Persons |
|---|---|---|---|
|
Number |
375 |
223 |
598 |
|
Rate (per 100,000) |
85 |
51 |
68 |
Note: Rates are crude per 100,000 population.
Source: AIHW National Hospital Morbidity Database.
Indigenous and non-Indigenous Australians
In 2021–22, Indigenous Australians were 3.1 times as likely as non-Indigenous Australians to be hospitalised due to a thermal injury (Table 4). Deaths are not compared here due to the small number of cases.
|
|
Males |
Females |
Persons |
|---|---|---|---|
|
Indigenous Australians |
78 |
46 |
62 |
|
Non-Indigenous Australians |
26 |
15 |
20 |
Notes
- Rates are age-standardised to the 2001 Australian population (per 100,000).
- ‘Non-Indigenous Australians’ excludes cases where Indigenous status is missing or not stated.
Source: AIHW National Hospital Morbidity Database.
The age-specific rate of injury hospitalisations due to thermal causes was highest among the 0–4 age group (Figure 5).
Figure 5: Hospitalisations for thermal injuries, by Indigenous status, age group and sex, 2021–22
Column graph for hospitalisations. The columns represent data for Indigenous and non-Indigenous Australians by 6 life-stage age groups. The reader can choose to display rate per 100,000 population or number. The reader can also choose to display data for persons, males, or females.
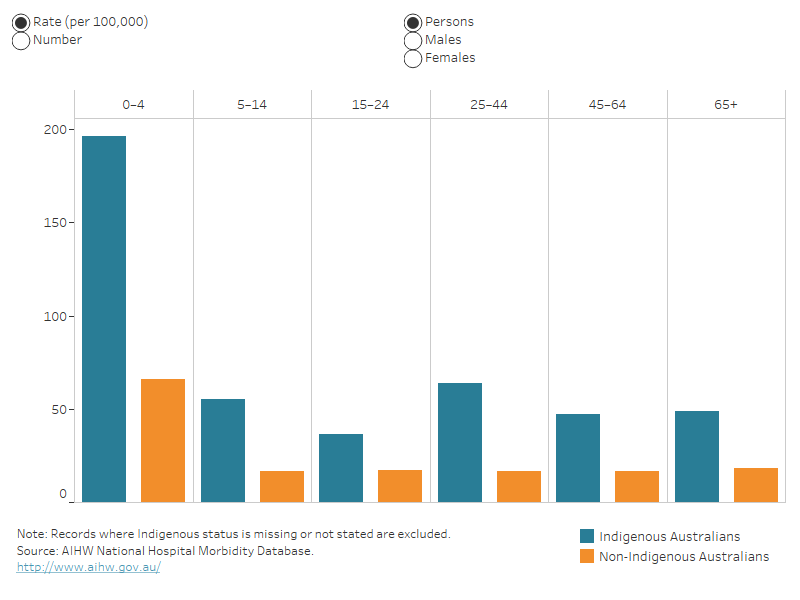
For more detail, see Data tables A4–A6 and D4–D8.
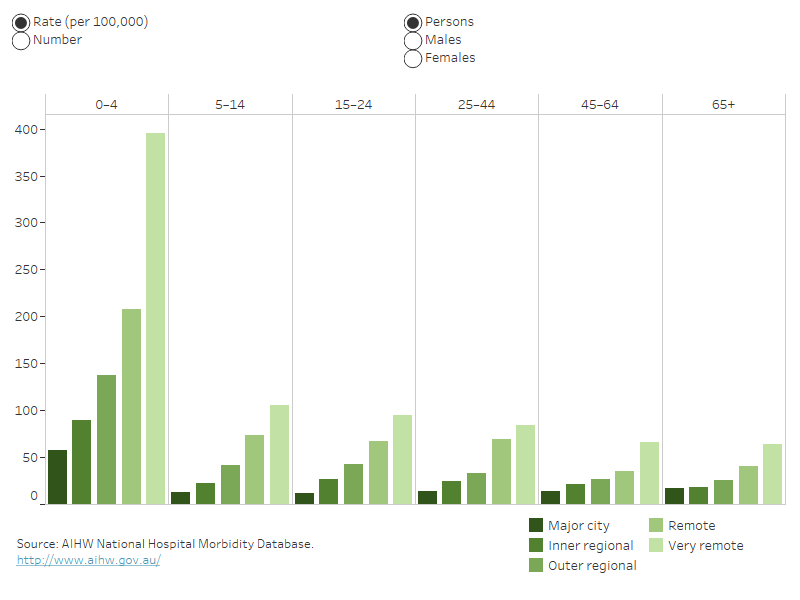
Remoteness
In 2021–22, people living in Very remote areas were 6.0 times as likely as people living in Major cities to be hospitalised for a thermal injury (Table 5).
Deaths data are not presented because of small numbers.
|
Males |
Females |
Persons |
|
|---|---|---|---|
|
Major cities |
20 |
13 |
17 |
|
Inner regional |
38 |
17 |
27 |
|
Outer regional |
57 |
23 |
40 |
|
Remote |
82 |
52 |
67 |
|
Very remote |
123 |
77 |
101 |
Note: Rates are age-standardised per 100,000 population.
Source: AIHW National Hospital Morbidity Database.
In 2021–22, when comparing remoteness areas, the rate of hospitalisation for thermal injuries was highest for children aged 0–4 living in Very remote areas (Figure 6).
Figure 6: Hospitalisations for thermal injuries, by remoteness, by age group and sex, 2021–22
Column graph for hospitalisations. The columns represent data for each of the 5 remoteness categories by 6 life-stage age groups. The reader can choose to display rate per 100,000 population or number. The reader can also choose to display data for persons, males, or females.
For more detail, see Data tables A7–A9 and D9–D10.
For information on how statistics are calculated by remoteness, see the technical notes.
Data details
Technical notes: how the data were calculated
Data tables: download the full tables
The following are recent publications that include information on thermal causes of injury. Search Reports for older publications.
- Data update: Short-term health impacts of the 2019–20 Australian bushfires, Burns
- Indigenous injury deaths, 2011–12 to 2015–16
- Hospitalised injury and socioeconomic influence in Australia, 2015–16
- Injury mortality and socioeconomic influence in Australia, 2015–16
- Hospitalised burn injuries Australia, 2013–14
ACCD (Australian Consortium for Classification Development) 2019. The international statistical classification of diseases and related health problems, 10th revision, Australian modification (ICD-10-AM), 11th ed. Tabular list of diseases and alphabetic index of diseases. Adelaide: Independent Hospital Pricing Authority (IHPA), Lane Publishing.
WHO (World Health Organization) 2016. International statistical classification of diseases and related health problems, tenth revision. 5th ed. Geneva: WHO.


