This represents 5.3% of hospitalised injuries and 0.2% of injury deaths.
In medical coding terms, this topic includes exposure to animate mechanical forces, contact with venomous animals and plants and exposure to or contact with allergens: allergy to animals.
Because of the low number of deaths from contact with living things, deaths are not described further.
This category only includes unintentional injuries. Intentional harm is included under Assault and homicide.
Causes of hospitalisation
In 2021–22:
- Contact with non-venomous animals was the top cause (60%) of hospitalisations in this category (Table 1). Of these, 56% involved dogs (Table 2)
- person-to-person contact accounted for 26% of hospitalisations in this category (Table 1)
- of the 7% of hospitalisations involving venomous animals, 27% of these were due to snakes (Table 3).
Table 1: Causes of injury hospitalisations due to contact with living things, 2021–22Cause | Hospitalisations | % | Rate (per 100,000) |
|---|
Contact with non-venomous animals (W53–59, W61) | 17,162 | 60 | 67 |
|---|
Unintentional person-to-person contact (W50–52) | 7,441 | 26 | 29 |
|---|
Contact with venomous animals and plants (X20-29) | 2,032 | 7 | 7.9 |
|---|
Allergy to animals (Y37.6) | 1,176 | 4.1 | 4.6 |
|---|
Contact with plants (W60) | 420 | 1.5 | 1.6 |
|---|
Other and unspecified (W64) | 238 | 0.8 | 0.9 |
|---|
Total | 28,469 | 100 | 111 |
|---|
Notes
1. Rates are crude per 100,000 population.
2. Percentages may not total 100 due to rounding.
3. Codes in brackets refer to the ICD-10-AM (11th edition) external cause codes (ACCD 2019).
4. Person-to-person contact includes being hit, struck, kicked, twisted, bitten or scratched by another person, striking against or bumping into another person, and being crushed, pushed or stepped on by crowd or human stampede. Injuries involving a fall because of a collision with or pushing by another person are not included. See Falls.
Source: AIHW National Hospital Morbidity Database.
Table 2: Non-venomous animals involved in injury hospitalisations, 2021–22Type of animal | Hospitalisations | % | Rate (per 100,000) |
|---|
Dogs (W54) | 9,542 | 56 | 37 |
|---|
Other mammals (W55) | 4,924 | 29 | 19 |
|---|
Non-venomous snakes, lizards and other reptiles (W59) | 1,829 | 11 | 7.1 |
|---|
Non-venomous insects and arthropods (including spiders) (W57) | 544 | 3.2 | 2.1 |
|---|
Non-venomous marine animals (excluding crocodiles) (W56) | 223 | 1.3 | 0.9 |
|---|
Birds (W61) | 52 | 0.3 | 0.2 |
|---|
Rats (W53) | 22 | 0.1 | 0.1 |
|---|
Crocodiles and alligators (W58) | 26 | 0.2 | 0.1 |
|---|
Total | 17,162 | 100 | 67 |
|---|
Notes
1. Rates are crude per 100,000 population.
2. Percentages and rate may not sum to total due to rounding.
3. Codes in brackets refer to the ICD-10-AM (11th edition) external cause codes (ACCD 2019).
Source: AIHW National Hospital Morbidity Database.
Table 3: Venomous animals involved in injury hospitalisations, 2021–22Type of venomous animal | Hospitalisations | % | Rate (per 100,000) |
|---|
Snakes (X20) | 539 | 27 | 2.1 |
|---|
Spiders (X21) | 474 | 23 | 1.8 |
|---|
Bees and wasps (X23) | 201 | 10 | 0.8 |
|---|
Others (X22, X24–X29) | 818 | 40 | 3.2 |
|---|
Total | 2,032 | 100 | 7.9 |
Notes
1. Rates are crude per 100,000 population.
2. Percentages may not sum to total due to rounding.
4. Codes in brackets refer to the ICD-10-AM (11th edition) external cause codes (ACCD 2019).
Source: AIHW National Hospital Morbidity Database.
For more detail, see Data tables B19–20.
Trends over time
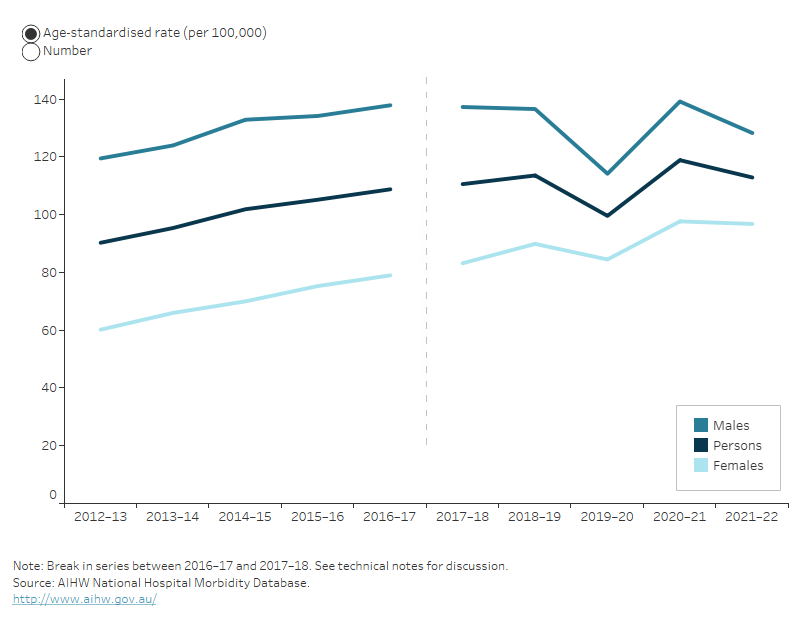
Over the period from 2017–18 to 2021–22, the age-standardised rate of hospitalisations due to contact with living things increased by an annual average of 0.5%. Figure 1 shows that this was largely driven by an increase among females. From 2012–13 to 2016–17 there was an average annual increase of 4.8%.
There is a break in the time series for hospitalisations between 2016–17 and 2017–18, due to a change in data collection methods (see the technical notes for details).
Figure 1: Injury hospitalisations due to contact with living things, by sex and year



 28,500 hospitalisations in 2021–22
28,500 hospitalisations in 2021–22 27 deaths in 2020–21
27 deaths in 2020–21