This represents 1.0% of injury hospitalisations and 0.9% of injury deaths.
This page summarises data on unintentional thermal injuries only. Intentional injuries and deaths are included under Assault and homicide or Self-harm and suicide.
Thermal causes of injury that led to hospitalisation
In 2021–22:
- 3 in 5 hospitalisations due to thermal causes (60%) were from contact with heat and hot substances
- 2 in 5 hospitalisations due to thermal causes (40%) were from exposure to fire, smoke and flames (Table 1).
Table 1: Thermal causes of injury that led to hospitalisation, 2021–22Cause | Hospitalisations | % | Rate (per 100,000) |
|---|
Contact with heat and hot substances (X10–19) | 3,352 | 60 | 13.1 |
|---|
Contact with hot drinks, food, fats and cooking oils (X10) | 1,010 | 18 | 3.9 |
|---|
Contact with hot fluids that are not hot drinks, food, fats and cooking oils (for example, water boiled on stove and hot tap water) (X11–12) | 1,043 | 19 | 4.1 |
|---|
Contact with hot household appliances, heating appliances, radiators and pipes (X15-16) | 536 | 9 | 2.1 |
|---|
Contact with hot engines, machinery and tools (X17) | 195 | 4 | 0.8 |
|---|
Other or unspecified (X13,X14,X18–19) | 568 | 10 | 2.2 |
|---|
Exposure to fire, smoke and flames (X00–09) | 2,192 | 40 | 8.5 |
|---|
Exposure to a controlled or uncontrolled fire (X00–03) | 901 | 16 | 3.5 |
|---|
Exposure to ignition of highly flammable material (X04) | 430 | 8 | 1.7 |
|---|
Other or unspecified (X05–09) | 861 | 16 | 3.3 |
|---|
Total | 5,544 | 100 | 21.6 |
|---|
Notes
- Rates are crude per 100,000 population.
- Percentages and rates may not equal total due to rounding.
- Codes in brackets refer to the ICD-10-AM (11th edition) external cause codes (ACCD 2019).
Source: AIHW National Hospital Morbidity Database.
For more detail, see Data tables B13–14.
In 2020–21, two thirds of deaths from thermal causes (66%) were from exposure to fire, smoke and flames (Table 2).
Table 2: Thermal causes of injury that led to death, 2020–21Cause | Deaths | % | Rate (per 100,000) |
|---|
Exposure to a controlled or uncontrolled fire (X00–03) | 64 | 54 | 0.2 |
|---|
Other or unspecified exposure to fire, smoke or flames (X04–09) | 15 | 13 | 0.1 |
|---|
Contact with heat and hot substances (X10–19) | 11 | 9 | 0.0 |
|---|
Elsewhere classified | 29 | 24 | 0.1 |
|---|
Total | 119 | 100 | 0.5 |
|---|
Notes
- Rates are crude per 100,000 population, calculated using estimated resident population as at 31 December of the relevant year.
- Percentages may not equal 100 due to rounding.
- Codes in brackets refer to the ICD-10 external cause codes (WHO 2011).
Source: AIHW National Mortality Database.
For more detail, see Data tables B19–21.
Trends over time
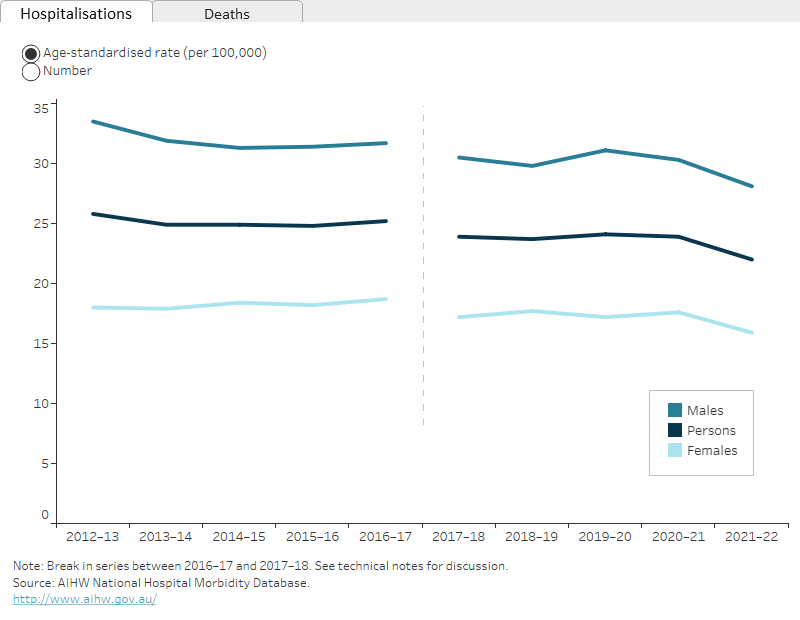
Over the period from 2017–18 to 2021–22, the age-standardised rate of hospitalisations for thermal injuries decreased by an annual average of 2.0%. From 2012–13 to 2016–17 there was an average annual decrease of 0.6%.
There is a break in the time series for hospitalisations between 2016–17 and 2017–18 due to a change in data collection methods (see the technical notes for details).
The rate of deaths from thermal injuries decreased between 2011–12 and 2020–21 by an annual average of 2.4% (Figure 1).



 5,500 hospitalisations in 2021–22
5,500 hospitalisations in 2021–22 120 deaths in 2020–21
120 deaths in 2020–21