People who inject drugs
Key findings
View the People who inject drugs fact sheet >
People who inject drugs are at increased risk of experiencing harms such as stigma and discrimination, fatal and non-fatal overdose, and blood-borne infectious diseases (such as HIV and hepatitis C). There were over 11 million people who inject drugs globally in 2020, of whom 1.4 million were living with HIV and 5.5 million with hepatitis C. Almost 1.2 million people live with both (UNODC 2022).
Prevalence of drug injection
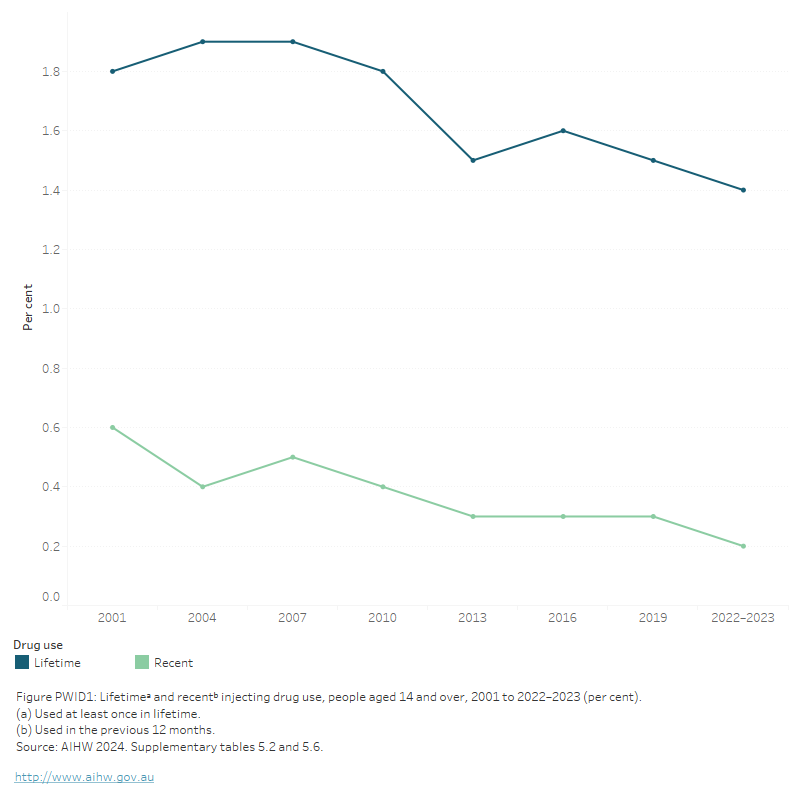
In Australia, a low proportion of the general population report injecting drugs. Information on data sources referred to in this section are in Box PWID 1. The National Drug Strategy Household Survey (NDSHS) found that in 2022–2023, 1.4% of the population aged 14 and over had injected a drug in their lifetime (AIHW 2024, Table 5.2), with 0.2% having injected a drug in the past year (both stable from 2019) (AIHW 2024, Table 5.6, Figure PWID 1).
Box PWID 1: Data sources examining drug use and harms among PWID
As people who inject drugs are likely to be underrepresented as respondents of the NDSHS, this section will largely draw upon data from other sources that are specifically targeted at people who inject drugs including the Illicit Drug Reporting System (IDRS) coordinated by the National Drug and Alcohol Research Centre (NDARC) and the Australian Needle and Syringe Program Survey (ANSPS) coordinated by the Kirby Institute.
Figure PWID 1: Lifetimea and recentb injecting drug use, people aged 14 and over, 2001 to 2019 (per cent)
The figure shows that both lifetime and recent injecting drug use were lower in 2019 than in 2001. Lifetime drug use decreased slightly from 1.8% of people aged 14 and over in 2001, to 1.5% in 2019. Similarly, recent drug use fell from 0.6% to 0.3%.
Illicit drugs
Heroin and methamphetamine are the most commonly injected drugs in Australia and are often cited as preferred drugs among people who inject drugs (Heard et al. 2023; Sutherland et al. 2023).
Estimates from the Illicit Drug Reporting System (IDRS) show that methamphetamine continues to be the most common drug of choice among people who inject drugs, after surpassing heroin in 2021, for the first time since monitoring began (Sutherland et al. 2023).
Drug most often injected
Estimates from the 2023 IDRS showed that, among participants who responded:
- Methamphetamine (56% of participants) and heroin (37%) were the most common drugs injected in the last month.
- The proportion of participants who said heroin was the drug they injected most often in the last month remained stable, 37% in 2023 and 35% in 2022. The proportion of participants who said methamphetamine was the drug they injected also remained stable, 56% in 2023 and 54% in 2022 (Sutherland et al. 2023, Figure 2).
- In the preceding 6 months, 80% of participants reported using crystal methamphetamine, with 96% of those participants reporting the main route of administration was injecting.
- Over half (56%) of the IDRS participants reported using heroin in the preceding 6 months, remaining stable relative to 2022 (53%), and represents an overall decline from 79% in 2000 (Sutherland et al. 2023, Figure 4).
- Of those participants who had recently used heroin, 34% reported using it daily (Sutherland et al. 2023).
IDRS data collection for 2023 took place in June and July. Changes due to the impacts of COVID-19 resulted in IDRS interviews in 2020–2023 being delivered face-to-face as well as via telephone and videoconference. All interviews prior to 2020 were delivered face-to-face, this change in methodology should be considered when comparing data from the 2020–2023 samples relative to previous years.
Last drug injected
Injecting drug use is often assessed by asking people to report the drug that they most recently injected (last drug injected). Data from the Australian Needle Syringe Program Survey 2018–2022 showed that methamphetamine and heroin are the most common last drugs injected (Figure PWID 2).
- In 2022, methamphetamine (47%) was the most commonly reported last drug injected nationally and across most jurisdictions (ranging from 29–67%). Nationally, this figure has decreased from 48% in 2018.
- Heroin (25%) was the second most commonly reported last injected drug in 2022. The proportion of respondents who reported last injecting heroin decreased from 26% in 2018.
- Performance and image enhancing drugs (PIEDs) was the third most commonly reported class of drugs last injected, with the proportion in 2022 (7%) higher than in 2018 (4%).
Other drugs that are often reported as the last drug injected include:
- Pharmaceutical opioids (including morphine, oxycodone, and fentanyl), (5% in 2022; 7% in 2018).
- Methadone (6% in 2022; 4% in 2018) (Heard et.al. 2023).
Figure PWID 2: Percentage of respondents by last drug injected, 2012 to 2022
The figure shows that in 2021, methamphetamine was the most common drug that was last injected (51%), followed by heroin (20%) and pharmaceutical opioids (7%). In 2021, 5% of respondents had last injected more than one drug.

Other frequently used drugs
Use of non-prescribed cannabis by people who inject drugs is also common. The 2023 IDRS showed that:
- Over two-thirds (69%) of participants had used non-prescribed cannabis in the last 6 months, relatively stable from 72% in 2022.
- Just over half (51%) of those who had recently used non-prescribed cannabis reported daily use, stable from 2022 (51%) (Sutherland et al. 2023).
People who inject drugs also use pharmaceutical drugs, particularly prescription opioids, at higher rates than the general population (Sutherland et al. 2023). This likely reflects the practice of substituting pharmaceutical drugs for illicit drugs, such as heroin. Data from the 2023 IDRS showed that, in the last 6 months:
- 10% of participants reported non-prescribed use of morphine.
- 10% reported non-prescribed use of oxycodone, stable from 10% in 2022.
- 9% reported non-prescribed use of buprenorphine-naloxone film, stable from 7% in 2022.
- 6% reported non-prescribed use of buprenorphine
- 6% reported non-prescribed use of fentanyl (Sutherland et al. 2023).
Use of cocaine is also relatively common among people who inject drugs, with 16% of participants in the 2023 IDRS reporting using cocaine in the last 6 months, stable from 15% in 2022 (Sutherland et al. 2023).
Health and harms
Injecting drug use is a major risk factor for transmitting blood-borne viruses, including HIV, hepatitis B and hepatitis C. Needle and syringe sharing among people who inject drugs is partly responsible for transmitting infection, although unsafe sexual behaviours also play a role (AIHW 2012).
Burden of disease and injury
The Australian Burden of Disease study, 2018, found that unsafe injecting practices were responsible for 0.9% of the total burden of disease and injuries in 2018 (AIHW 2021).
Unsafe injecting practices are linked to Hepatitis B, Hepatitis C, HIV/AIDS, liver cancer and chronic liver disease. Liver cancer and chronic liver disease are the long-term consequences of contracting hepatitis B and hepatitis C infection. Acute hepatitis C and B were responsible for 74% and 33% of burden (respectively) (AIHW 2021). Chronic liver disease and liver cancer were each responsible for 27% of the burden due to unsafe injecting practices (AIHW 2021).
The IDRS report on trends in self-reported past year non-fatal overdose and responses to overdose found that, between 2009 and 2020, the proportion of participants who reported receiving no treatment on the occasion of their overdose fluctuated but remained above 10% (Thomas et al. 2021).
Injecting risk behaviours
Data from the Australian Needle Syringe Program Survey (ANSPS) provides some evidence of the risk of harms related to injecting drug use in people who regularly inject drugs in Australia:
- The proportion of respondents reporting recent reuse of needles and syringes (including the reuse of one’s own syringes) was stable over the past 5 years (from 23% in 2018 to 26% in 2022).
- The proportion of respondents reporting receptive sharing of needles and syringes in the last month was stable over the past 5 years (from 16% in 2018 to 19% in 2022) (Heard et al. 2023).
Data from the 2023 IDRS provide additional evidence of risks for harms, including:
- 7% of participants reported lending a needle to someone after they had used it, and 5% reported borrowing a needle after someone else had used it.
- 1 in 3 (33%) participants reporting re-using their own needle in the last month.
- 1 in 5 (21%) participants reporting sharing other injecting equipment (for example, spoons) in the last month, stable relative to 2022 (20%) and down from a high of 51% in 2000 (Sutherland et al. 2023, Figure 35; Figure PWID 3).
Figure PWID 3: Injecting risk behaviours in the last month among people who inject illicit drugs, 2000 to 2022 (per cent)
The figure shows that injecting risk behaviours have fluctuated between 2000 and 2022. Re-use of own needles overall decreased from 53% in 2008 to 33% in 2022. Borrowing needles fell from 16% in 2000 to 5% in 2022, though lending of needles remained relatively stable (11% in 2000 and 7% in 2022). Sharing of other equipment decreased from 51% in 2000 to 5% in 2019, before increasing to 21% in 2022.

Injection-related health problems
In 2023, 26% of IDRS participants reported experiencing an injection-related health problem in the last month stable from 2022 (26%). Of those who responded (n=817), in the last month:
- 10% experienced nerve damage, similar to 2022 (11%).
- 6% reported that they had experienced a ‘dirty hit’ (that is, a hit that made them feel sick), similar to 2022 (7%).
- 10% experienced an infection or abscess, similar to 2022 (12%) (Sutherland et al. 2023, Table 20).
National HIV antibody prevalence is low. The ANSPS found that among survey participants, there was a slight increase in prevalence from 1.7% in 2018 to 2.1% in 2022 (Heard et al. 2023; Table 1.2.1). Some people are at greater risk of HIV than others.
- Nationally, across all survey years, HIV antibody prevalence was consistently higher among male respondents than female respondents (Figure PWID 4). HIV antibody prevalence has also been consistently higher among homosexual male respondents (37.9%) than among bisexual (2.8%) and heterosexual (0.3%) male respondents (Heard et al 2023; Table 1.2.2).
- Between 2018 and 2022, HIV prevalence was also higher among those who reported methamphetamine as the last drug injected (3.1% in 2022) compared to those who reported last injecting other drugs (0.9% for heroin as the last drug injected and 0.5% for those with other opioids as the last drug injected) (Heard et al; Table 1.2.4).
- HIV prevalence was similar among those aged 45 years and over (2.4% in 2022) and those aged 35–44 years, 0.8% of people aged 25–34 and 0% for those under 25 years (Heard et al. 2023; Table 1.2.3).
Figure PWID 4: HIV antibody prevalence by sex, 1995 to 2022 (per cent)
This figure shows that HIV antibody prevalence has fluctuated across time and was lower in 2021 (1.5% of persons) than 2020 (2.5%). HIV antibodies have typically been more prevalent among males (1.8% in 2021) than females (0.6% in 2021).

According to the ANSPS, Hepatitis C (HCV) is more common than HIV among PWID. Almost 1 in 3 (32%) of respondents were HCV antibody positive in 2022, a decline from 45% in 2018 (Heard et al. 2023, Table 1.3.1).
- HCV antibody prevalence was higher among older respondents and those with longer injection histories.
- Prevalence of HCV antibodies continues to be higher among respondents reporting heroin or other opioids as the last drug injected (both 45%) compared to respondents who last injected methamphetamine (27%).
- HCV RNA prevalence (active infection) was consistently higher among respondents who reported imprisonment in the year preceding survey completion compared to those who had not been incarcerated.
- HCV RNA prevalence was also consistently higher among respondents who reported receptive needle and syringe sharing in the last month compared to respondents who did not report receptive sharing.
- HCV Direct Acting Antiviral (DAA) therapy was included on the Australian Government Pharmaceutical Benefits Scheme (PBS) from March 2016. Lifetime HCV treatment, among respondents eligible for treatment only, increased from 55% in 2018 to 68% in 2022 (Heard et al. 2023).
Data collection for the 2021 ANSPS was impacted by COVID-19 restrictions. The survey took place in several phases from September to December 2021, instead of the usual October timeframe. Victoria and NSW experienced outbreaks between June and November 2021, resulting in a reduction in the amount of participating NSP services. This should be taken into account when comparing data from 2021 with previous years.
Treatment
Data from the 2023 IDRS found that:
- Nearly 2 in 5 (39%) participants reported receiving treatment for substance use in 2023, similar to 2022 (38%). The most common treatment was methadone (21% of participants) (Sutherland et al. 2023, Table 21).
- Fourteen per cent of participants reported difficulties accessing treatment in the last 6 months. Methamphetamine (43%) and heroin (42%) were the main substances for which these participants had last sought treatment (Chandrasena et al. 2024).
Policy context
For related content on policy related to injecting drug use, see also:
Policy support
The 2022–2023 NDSHS showed that most people support measures to reduce harms associated with injecting drugs. Specifically:
- Over two-thirds of the population aged 14 and over supported methadone/buprenorphine maintenance programs (71%).
- 68% supported needle and syringe programs.
In addition:
- A trial of prescribed heroin received the least support (35%).
- Aside from a trial of prescribed heroin and use of naltrexone, higher proportions of females than males supported measures aimed at reducing harms associated with injecting drug use (AIHW 2024, Table 11.21)
Needle and syringe programs
All Australian states and territories operate needle syringe programs (NSPs), providing a range of services to people who inject drugs (Heard et al. 2022). See Harm reduction: Minimising risky behaviours
According to the IDRS, in 2017, NSPs were by far the most common source of needles and syringes in the preceding 6 months (94%), followed by NSP vending machines (19%). Chemists were used by 16% of participants nationally (Karlsson & Burns 2018, Table 51).
This is supported by the findings of the 2022–2023 NDSHS that NSPs were the most commonly reported source of needles and syringes (45%), followed by chemists (31%) (AIHW 2024, Table 5.110). This is likely to reflect the different sampling of the 2 surveys whereby the NDSHS is targeted at the general population, while the IDRS specifically recruits people who inject drugs.
Medically supervised injecting centres
Medically supervised injecting centres (MSIC) are places where people can use and inject drugs under the supervision of registered nurses, counsellors and health education professionals. This service aims to prevent injury and death by being present when someone injects in order to provide immediate medical assistance as required. Kings Cross in Sydney has been home to an MSIC since 2001 (Uniting 2017), and a second opened in Richmond, Victoria in July 2018.
AIHW (Australian Institute of Health and Welfare) (2012) Australia’s health 2010. Australia’s health series no. 12. Cat. no. AUS 122. Canberra: AIHW.
AIHW (2021) Australian Burden of Disease Study: Impact and causes of illness and death in Australia 2018, AIHW, Australian Government. doi:10.25816/5ps1-j259.
AIHW (2024) National Drug Strategy Household Survey 2022–2023. AIHW, accessed 29 February 2024.
Chandrasena U, Sutherland R & Peacock A (2024) Difficulty accessing drug treatment among a national sample of people who regularly inject drugs, Australia, 2023, National Drug and Alcohol Research Centre, UNSW Sydney, accessed 14 June 2024.
Heard S, Zolala F, Maher L, (2023) Australian Needle Syringe Program Survey. National Data Report 2018–2022. Sydney: Kirby Institute, UNSW Sydney. Viewed 14 August 2023.
Karlsson A & Burns L (2018) Australian Drug Trends 2017. Findings from the Illicit Drug Reporting System (IDRS). Australian Drug Trend Series. No. 181. Sydney, National Drug and Alcohol Research Centre, UNSW Australia.
Sutherland R, Uporova J, King C, Chandrasena U, Karlsson A, Jones F, Gibbs D, Price O, Dietze P, Lenton S, Salom C, Bruno R, Wilson J, Agramunt S, Daly C, Thomas N, Radke S, Stafford L, Degenhardt L, Farrell M, & Peacock A (2023) Australian Drug Trends 2023: Key Findings from the National Illicit Drug Reporting System (IDRS) Interviews. Sydney: National Drug and Alcohol Research Centre, UNSW Sydney; Accessed 25 October 2023.
Thomas N, Juckel J ,Daly C, Maravilla J & Salom C R (2021) Trends in self-reported past year non-fatal overdose and responses to overdose: Findings from the Illicit Drug Reporting System. Sydney. National Drug and Alcohol Research Centre, UNSW.
UNODC (United Nations Office on Drugs and Crime) (2022) World Drug Report 2022. Vienna: UNODC. Accessed 6 July 2022.
Uniting (2017) Uniting Medically Supervised Injecting Centre: get to know our story. Viewed 25 January 2018.


