Chronic conditions and burden of disease
Data updates
25/02/22 – In the Data section, updated data related to chronic conditions and burden of disease are presented in Data tables: Australia’s children 2022 - Health. The web report text was last updated in December 2019.
Key findings
- For 2017–18, asthma, hay fever and allergic rhinitis, anxiety-related problems and psychological development problems were the 4 leading chronic conditions for children aged 0–14, based on self-reported proxy data from the ABS National Health Survey.
- Among all children aged 5–14, asthma was the leading cause of disease burden followed by mental health disorders.
Chronic conditions, also known as long-term conditions or non-communicable diseases, refers to a wide range of conditions, illnesses and diseases that tend to be long lasting with persistent effects.
Chronic conditions can interrupt a child’s normal development and can increase their risk of being developmentally vulnerable at school entry (Bell et al. 2016). Because chronic conditions often persist throughout a person’s life, there is generally a need for long-term management by individuals and health professionals (AIHW 2018a).
Managing chronic conditions can be complex, expensive and take a psychological, social and economic toll on the children affected and their families. Early intervention and joined-up support services can minimise the negative effects and support families (AHMAC 2015).
Burden of disease analysis measures the impact of different diseases or injuries on a population. This is done by measuring how many years of life Australia loses to diseases either due to people:
- dying early (fatal burden)
- living with ill health (non-fatal burden) (AIHW 2018b).
This section provides an overview of chronic conditions among children and the leading causes of the total burden of disease. Separate sections of this report focus on 4 specific chronic conditions that can have a major impact: asthma, diabetes, cancer and mental health conditions. These conditions significantly impact children’s lives and are leading causes of disease burden (asthma, mental health conditions) (Figure 2), particularly common among children (Type 1 diabetes) (see Children with Diabetes), or a leading cause of death (cancer) (see Cancer incidence and survival).
In 2017–18, around 43% of children had at least 1 long-term condition, while 20% had 2 or more long-term conditions. Boys were more likely to have at least 1 long-term condition than girls (46% compared with 39%) (ABS 2019b).
There are socioeconomic differences in the prevalence of some conditions, but this varies depending on if the disease risk factors/etiology are related to socioeconomic drivers. However, ensuring there is equity with service use and access is important for the treatment and/or management of chronic conditions.
What are the most common chronic conditions?
Based on self-reported data from the ABS National Health Survey 2017–18, the 2 leading chronic conditions for children aged 0–14 were diseases of the respiratory system:
- asthma
- hay fever and allergic rhinitis, both 10% (Figure 1).
Both these diseases are more common among people with hypersensitivity to allergens. For more information on asthma, see Asthma prevalence among children.
The third and fourth leading conditions relate to mental and behavioural disorders:
- anxiety-related problems
- psychological development problems—5.7% for each).
For more information on mental health, see Children with mental Illness and Social and emotional wellbeing.
The fifth most commonly reported chronic condition was food allergies (5.5%). In Australia, a 350% increase in hospital admissions for anaphylaxis and food allergies was reported in 1994–95 to 2004–05 (AHMAC 2015).
The number of children with a food allergy or food-related immune disorder has increased in the last 10 years. A study of more 2,000 Melbourne infants (the Healthnuts study) found that more than 10% of 1 year olds have a food allergy. Common food allergies, such as egg and milk allergies, which were previously limited to early childhood, are becoming increasingly persistent (Osborne et al. 2011).
Vision disorders are also common among children, with around 12% of children experiencing a vision disorder (diseases of the eye and adnexa) (ABS 2019a). The most common long-term vision disorders were short-sightedness (4.5% of children) and long-sightedness (4.3%) (Figure 1). Recent research on short-sightedness showed that increasing the time that children spend outside can slow the onset of short-sightedness (Morgan & Rose 2019).
Figure 1: Most commonly reported long-term conditions in children aged 0–14, 2017–18
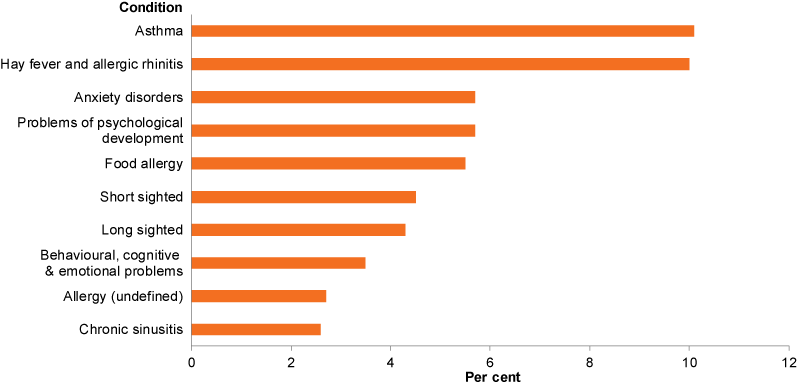
Note: Long-term condition is defined here as a condition which has lasted, or is expected to last, for 6 months or more.
Source: ABS 2019a.
A study based on data from the Longitudinal Study of Australian Children (LSAC) looked at the prevalence and persistence of 19 paediatric conditions among the same group of children from infancy to mid-adolescence (aged 14–15). The paediatric conditions discussed in this study are defined differently to the chronic conditions discussed earlier in this section. Most children (60%) were found to have at least 1 ongoing health condition at any given time, although many of the conditions discussed resolved within 2 years.
The prevalence of 8 paediatric conditions rose steadily with age:
- overweight/obesity
- obesity
- injury
- anxiety/depression
- frequent headaches
- abdominal pain
- autism spectrum disorder
- attention-deficit hyperactivity disorder.
The prevalence of 6 conditions fell with age:
- eczema
- sleep problems
- day-wetting
- soiling
- constipation
- recurrent tonsillitis.
Three conditions remained stable (asthma, diabetes, epilepsy) and 2 peaked in mid-childhood (dental decay, recurrent ear infections).
Conditions were more likely to persist through childhood if present for 2 years; persistence was especially high for obesity beyond those aged 6–7 (91%–95%) persisting to the ages of 14–15. (Liu et al. 2018).
What are the leading causes of the burden of disease?
In 2015, findings from the Australian Burden of Disease Study 2015, reported that for children under the age of 5, 4 of the 5 leading causes of the total burden of disease were infant and congenital conditions, mostly due to pre-term birth and low birthweight complications (see Infant and child deaths) (Figure 2).
Among all children aged 5–14, asthma was the leading cause of burden followed by mental health disorders and dental caries (Figure 2).
Figure 2: Leading causes of total burden among children aged 0–14, by age group, 2015
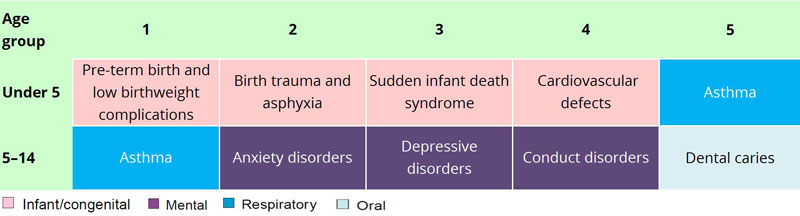
Note: Excludes ‘other’ residual conditions.
Source: AIHW Burden of Disease database.
In 2015, asthma and anxiety disorders were the 2 leading causes of burden among boys and girls aged 5–14. For boys the third leading cause of burden was conduct disorders, while for girls it was depressive disorders (AIHW 2019).
In 2011, findings from the Australian Burden of Disease Study 2011 (which included estimates for the Indigenous population) showed that among Indigenous children aged 5–14, 4 of the 5 leading causes of the disease burden were the same as those for all children in 2015 although the order differed. Conduct disorder was the first leading cause followed by asthma (Figure 3).
Figure 3: Leading causes of total burden among Indigenous children aged 0–14, by age group, 2011
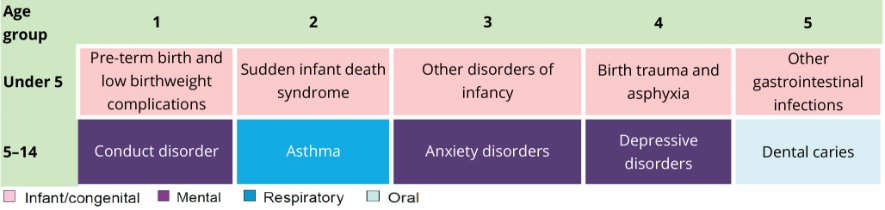
Source: AIHW Burden of Disease database.
Conduct disorder and asthma were the 2 leading causes of burden among Indigenous boys aged 5–14. For Indigenous girls, the 2 leading causes of burden were asthma and anxiety disorders (AIHW 2016).
Data limitations and development opportunities
Future reporting of priority populations may be possible with linkage. For more information, see Data gaps.
ABS (Australian Bureau of Statistics) 2019a. National Health Survey: first results, 2017–18. ABS cat. no. 4363.0.55.001. Canberra: ABS.
ABS 2019b. Microdata: National Health Survey 2017–18. ABS cat. no. Findings based on Detailed Microdata analysis.
AHMAC (Australian Health Ministers’ Advisory Council) 2015. Healthy, safe and thriving: national strategic framework for child and youth health. Adelaide: AHMAC. Viewed 17 May 2019.
AIHW (Australian Institute of Health and Welfare) 2016. Australian Burden of Disease Study: impact and causes of illness and death in Aboriginal and Torres Strait Islander people 2011. Australian Burden of Disease Study series no. 6. Cat. no. BOD 7. Canberra: AIHW.
AIHW 2018a. Australia’s health 2018. Australia’s health series no. 16. Cat. no. AUS 221. Canberra: AIHW.
AIHW 2018b. Australia’s health 2018: in brief. Cat. no. AUS 222. Canberra: AIHW.
AIHW 2019. Australian Burden of Disease Study: impact and causes of illness and death in Australia 2015. Australian Burden of Disease series no. 19. Cat. no. BOD 22. Canberra: AIHW.
Bell MF, Bayliss DM, Glauert R Harrison A & Ohan JL 2016. Chronic illness and developmental vulnerability at school entry. Pediatrics 137(5):e20152475.
Liu T, Lingam R, Lycett K, Mensah F, Muller J, Hiscock H et al. 2018. Parent-reported prevalence and persistence of 19 common child health conditions. Archives of Disease in Childhood 103:548–556. doi:10.1136/archdischild-2017-313191.
Morgan IG & Rose KA 2019. Myopia: is the nature-nurture debate finally over? Clinical and experimental optometry 102:3–17.
Osborne NJ, Koplin JJ, Martin PE, Gurrin LC, Lowe AJ & Matheson MC 2011. Prevalence of challenge-proven IgE-mediated food allergy using population-based sampling and predetermined challenge criteria in infants. Journal of Allergy and Clinical Immunology 127(3):668–676.
National Health Survey 2017–18
- For technical information on the National Health Survey 2017–18, see: Explanatory Notes in National Health Survey: First Results, 2017-18
- For information on data quality, see: the National Health Survey 2017–18 Quality Declaration - Summary
Australian Burden of Disease Study 2015
- For information on the Australian Burden of Disease Study 2015, see: the methods and supplementary material
For more information, see Methods.


